Genetic analyses improve the detection and diagnosis of childhood cancers.

Camp Fantastic (CF), a week-long adventure at which Dr. Jack Shern serves as lead physician, lets children with cancer and neurofibromatosis “just be kids.” Since 1983, the camp has offered outdoor activities, and since COVID, virtual offerings like crafting and online science. Pictured clockwise from top left: Travis Carpenter creates paper flowers at Virtual CF 2020; Ryan Kovacs launches a water balloon at CF 2019; (from left) Taylor Caquias, Dominic Ortega, Tsadet Brannon, Campbell Brandt and Carolyn Shaffer enjoy some teen time at CF 2019; Abby Furco flanked by CF 2018 staff K School (left) and Sarah Rostock (right); and Becca Chamberlain goes horseback riding at CF 2019. CF is a partnership between the National Cancer Institute (NCI) and Special Love, Inc., a Northern Virginia charity that also provides programming and financial assistance for siblings and young adults. “It’s wonderful that the NCI can provide a safe environment where patients and survivors can feel normal and connect to other kids who understand what they’re going through,” says Shern. Credit: Special Love, Inc.; iStock
Genetic analyses have become a critical part of many cancer diagnoses, and CCR scientists are seeking to expand the impact of this technology. They have teamed up with colleagues around the world to pore over DNA from patient samples, looking for patterns that reveal the presence of cancer or hint at the future behavior of a tumor. Their recent discoveries could lead to more personalized treatments for patients with the childhood cancer rhabdomyosarcoma and more reliable cancer screenings for people with another childhood condition, neurofibromatosis type 1 (NF1).
Children diagnosed with rhabdomyosarcoma, a cancer that begins in the cells that give rise to muscle tissue, are usually treated with a combination of chemotherapy, radiation and surgery. Doctors use clinical features, such as the size and location of tumors, to determine how aggressive this treatment should be. These criteria are good at identifying patients whose risk of poor outcomes is particularly high or low, but most patients fall somewhere in between, where outcomes are difficult to predict.
New findings from the largest-ever international study on rhabdomyosarcoma, led by Senior Investigator Javed Khan, M.D., and Lasker Clinical Research Scholar Jack Shern, M.D., will help clinicians refine their diagnoses and offer patients more personalized treatment plans. The CCR team and collaborators at the Institute for Cancer Research in London, U.K., analyzed DNA from the tumors of more than 600 children with rhabdomyosarcoma, focusing on 39 genes linked to the disease.
They discovered that outcomes tended to be worse for patients whose tumors had mutations in a small handful of genes, including TP53, MYOD1 or CDKN2A, as reported in the Journal of Clinical Oncology. Additionally, patients with more than one mutation that drive cancer progression fared particularly poorly. This information is now guiding the design of clinical trials and will help in the development of new experimental therapies.
Another application that is quickly becoming useful in diagnosing and monitoring pediatric patients is the genomic profiling of circulating tumor DNA. Shern collaborated with a team at Washington University School of Medicine in St. Louis, led by assistant professors Angela Hirbe, M.D., Ph.D., and Aadel Chaudhuri, M.D., Ph.D., to analyze DNA isolated from the blood of people with NF1 in search of a better way to detect malignant tumors. NF1 is a condition that can cause large growths to develop along nerves throughout the body. Most of these remain benign, but sometimes they turn into aggressive cancers, and even with regular MRI (magnetic resonance imaging) scans, it can be difficult to spot those that do.
Jack F. Shern, M.D.
Lasker Clinical Research Scholar
Pediatric Oncology Branch
Javed Khan, M.D.
Deputy Chief
Genetics Branch
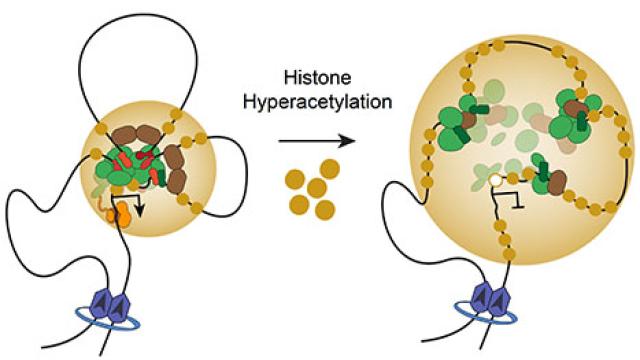
Shern’s team focused on DNA shed by cells into the blood, which included short fragments from tumor cells. When they sequenced the circulating DNA and compared the results of patients who had benign NF1 tumors to those from patients with malignant tumors, they found several features that set them apart.
The discovery, reported in PLOS Medicine, suggests it may be possible to distinguish between benign and malignant tumors in patients with NF1 with a simple, non-invasive blood test. Because the amount of tumor DNA in the blood dropped when patients’ malignant tumors shrank following treatment, a liquid biopsy might also be used to monitor how patients respond to therapy.
Khan and Shern are eager to see these genomic profiling tools move out of the lab to become routine for pediatric patients and help people with rhabdomyosarcoma and NF1.