A new method makes therapeutic cancer vaccines more reliably effective in mice.
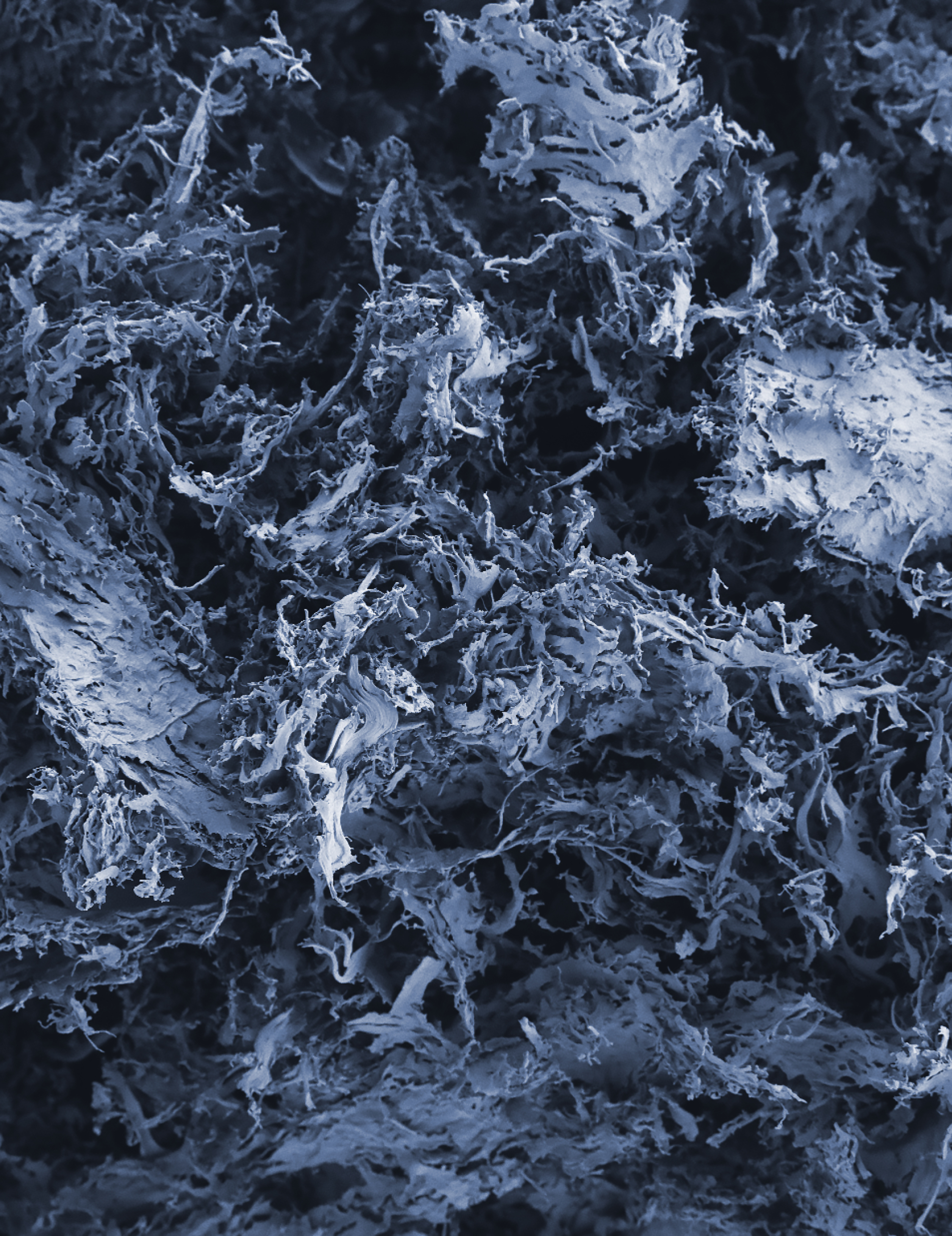
CCR researchers developed a biocompatible, porous and degradable scaffolding — seen here imaged with a scanning electron microscope — using the cell-free extracellular matrix of small intestine tissue. The biomaterial scaffolding can be implanted in the body where it will be remodeled into, and support the growth of, new tissue to repair injury by recruiting immune cells to the site. CCR researchers leveraged these properties to create a biocompatible scaffold-assisted therapeutic cancer vaccine that enhanced vaccine efficacy and eliminated tumors in mice and generated protective anti-cancer memory. This immunotherapy-infused scaffold could one day be implanted in patients to help prevent tumors from coming back after surgery.
Credit: Iris Baurceanu and Adam Harned, CCR, NCI, NIH; SPGM, FNL, NCI, NIH
Cancer therapies aren’t always drugs alone. Fighting cancer can involve multiple therapeutic approaches with fusions of new and existing treatments. In one such innovation, CCR researchers have developed a novel treatment that unites an existing surgical practice and tissue engineering with targeted therapeutic cancer vaccines. The combination caused tumor regression and provided a long-lasting anti-cancer immune response in mice.
Surgeons often use biomaterials to reconstruct or reinforce tissue after an operation; these materials can range from plastics to collagen. For example, when doctors remove a tumor, biomaterials can act as a scaffolding to fill the empty space left behind or support nearby structures in the body. Depending on their physical and chemical composition, these biomaterials also can initiate and regulate inflammation, a key process in how the immune system protects us from cancer.
“These biomaterials work well in a post-surgery environment, particularly because you can choose a material that facilitates healing by recruiting immune cells to repair the surgical wound,” says Stadtman Tenure-Track Investigator Matthew Wolf, Ph.D. He was curious to know if he could take advantage of the biomaterials and the unique immune cells that they summon to create an environment additionally suited to fighting cancer cells.
Wolf came up with the idea that therapeutic cancer vaccines might help to redirect the immune response from the biomaterials towards a specific cancer. While preventive vaccines prepare the healthy immune system to protect against viruses and bacteria, therapeutic cancer vaccines train the immune system to recognize and remember cancer cells that might have been left behind or start growing again after tumor removal.
In their study, published in Advanced Materials, Wolf’s team infused their biomaterial scaffolding with a therapeutic cancer vaccine cocktail that activates cytotoxic T lymphocytes, a type of cancer-fighting immune cell. Their design was engineered so that the scaffold would generate cancer-killing T cells in concert with the vaccine trapped within it, so the vaccine stayed at the site and did its work for longer rather than dissipating.
The result? An environment rich with immune cells, where the therapeutic cancer vaccine helps them effectively target tumor cells for longer than usual.
“Both the vaccine and the scaffold are providing unique parts of this immune response to turn into something that's greater than the sum of the two,” says Wolf. The researchers tested their therapy in mice with lymphoma tumors. The scaffold-enhanced cancer vaccine was able to stimulate the immune system to eradicate 50 to 75 percent of existing tumors. Months later, more tumors were introduced into the mice, and their immune systems successfully eradicated the new tumors too. This indicates that the treatment created a long-lasting immune memory, something Wolf and his colleagues are excited about.
“CCR’s extensive preclinical facilities made it possible for us to follow the animals for nearly a year so that we could show the longevity of our treatment,” says Wolf. “Our method is also convenient because it uses biomaterials that fit into normal surgical approaches to removing cancer; it may usher in an era that combines cancer immunotherapy treatment with regenerative medicine of surgical trauma.”