Having more diverse HLA genes is better for immune control of HIV.

When you have a variety of screwdriver heads in different sizes and shapes, you are more likely to find a precise match for a certain screw. Similarly, when you inherit different HLA genes from your parents, you are more likely to be able to display different viral proteins for your immune system to recognize. Having more ways to identify viruses makes the immune system more likely to mount a robust attack and keep viral loads in check in diseases such as HIV.
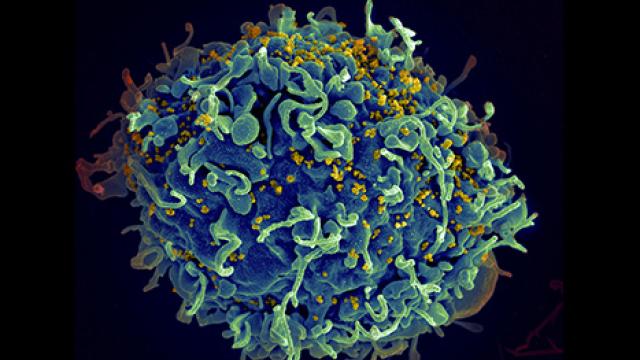
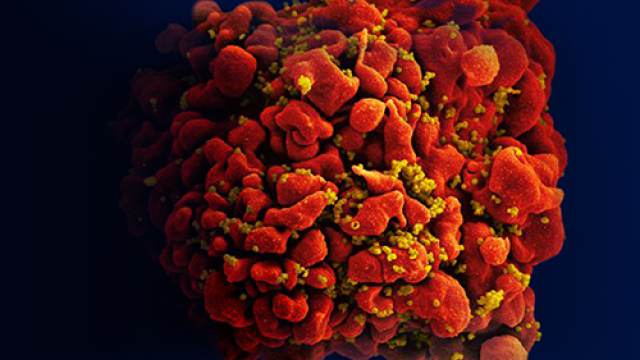
Credit: SPGM, FNL, NCI, NIH; iStock
More than 39 million people around the world live with HIV. While antiretroviral therapy can control the disease, not everyone can access these lifesaving treatments, and new advances are needed to end the ongoing AIDS pandemic. To develop new methods of both prevention and treatment, it is essential to understand how the immune system responds to HIV on its own. At CCR, scientists led by Senior Investigator Mary Carrington, Ph.D., have a newly detailed grasp of why some people’s immune systems do a better job of controlling the virus than others.
Before antiretroviral therapy was available, some patients developed AIDS soon after they became infected with HIV. Others lived for years with low levels of the virus in their blood. These disparities can be explained in part by differences in proteins called human leukocyte antigens (HLAs), which infected cells use to alert the immune system to the threat. HLAs sit on the surface of cells and display bits of the virus called peptides for surveilling immune cells to recognize as foreign.
When people inherit identical copies of an HLA gene from each parent, their immune system is less equipped to fight HIV than if their HLA genes were different. That is likely because having only one version limits which fragments of the virus can be displayed on the surface of an infected cell. With different HLA proteins, infected cells can present more diverse pieces of the virus, giving the immune system more ways to recognize the infected cells as targets.
The genes that encode HLAs are the most diverse genes in the human genome. While it is uncommon to have two copies that are an exact match, some mismatched pairs are more alike than others. Carrington wanted to know just how different HLA genes must be to improve viral control.
In work reported in Science, Carrington’s team cataloged how different pairs of HLA genes complement or overlap one another in displaying peptides to the immune system. “We're asking, ‘How similar are you? Do you bind primarily the same peptides with just slight differences? Or are you way over on the other end of the spectrum, where you're really recognizing completely separate types of peptides?’” Carrington explains. Using data from researchers at the Dana Farber Cancer Institute who had tested this peptide binding, her group came up with a measure of functional divergence for every possible pair of HLA genes.
Then they compared this functional divergence to clinical data. They looked for relationships between HLA diversity and patients’ viral load or the time it took untreated patients to develop AIDS after they became infected.
They found a clear association: People whose two HLA genes enabled their immune system to recognize very different fragments of viral proteins were better able to control the virus than people whose HLAs were very similar.
Carrington says she suspects HLA functional diversity probably affects individuals’ ability to control many kinds of infections, not just HIV. It may even influence patients’ response to vaccines and cancer immunotherapies. Her team’s measures of functional divergence will help researchers investigate these relationships, which could one day inform personalized treatment or prevention strategies for many diseases, including cancer.