Major prognostic and treatment advances are made against a rare and deadly disease.

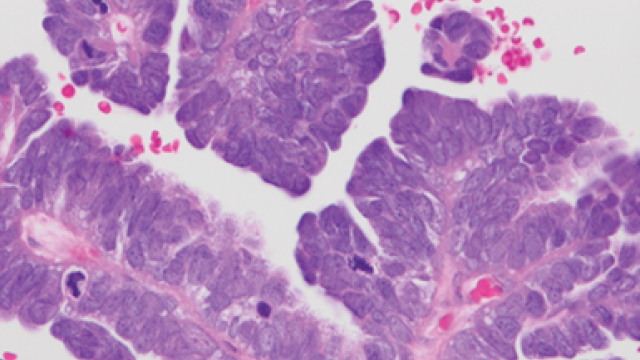
In one study, CCR researchers identified gene signatures that are associated with mesothelioma prognosis and can help determine a patient’s response to therapy. In a second study, CCR researchers showed that it was possible to treat mesothelioma with adoptive T-cell therapy. These two strikes against mesothelioma, one from basic research, one from a clinical trial, will help fight this rare cancer. Credit: iStock
Mesothelioma, an aggressive tumor that affects the lining of the lungs or abdomen, belongs to the unfortunate list of cancers that are aggressive, difficult to treat and have poor outcomes. But a combination of lab and clinical work in CCR now holds promise for a cancer that has been intractable for many years.
“The standard therapy for patients with mesothelioma is immunotherapy and chemotherapy,” says Raffit Hassan, M.D., who has been studying mesothelioma at CCR for decades. “But the median overall survival has been less than two years.” Recently, however, his team uncovered genetic signatures that hint at a patient’s prognosis and potential treatments, while results from a clinical study showed that a novel adoptive T-cell therapy can lead to tumor regression in some patients with treatment-resistant mesothelioma.
In one study, published in Cell Reports Medicine, Hassan and his colleagues analyzed blood and tumor samples of 122 mesothelioma patients and identified a group of 48 genes in which high expression was associated with worse survival. Higher expression of one gene in particular, CCNB1, which is involved in the growth of cells, was associated with significantly lower survival.
Then, in collaboration with Senior Investigator Eytan Ruppin, M.D., Ph.D., they used a computational tool Ruppin’s lab had developed, called SELECT, which analyzes the unique genetic makeup of a person’s cancer to predict which existing drugs could potentially be an effective treatment for that individual. Using the tool, the researchers were able to predict with high accuracy which patients would have a partial or complete response to seven different immunotherapy and chemotherapy drugs.
In a second study, Hassan and his colleagues reported results from a phase 1 clinical trial exploring the safety and efficacy of a novel cell therapy called gavocabtagene autoleucel (gavo-cel), developed by the immuno-oncology company TCR2 Therapeutics, now combined with Adaptimmune. The approach involves taking a patient’s T cells, a type of immune cell, and modifying them so that they recognize the mesothelin protein, which is highly expressed on mesothelioma. With their ability to target the cancer boosted, the modified T cells are then infused back to the patient.
As reported in Nature Medicine, the study included 32 patients with either mesothelioma or advanced mesothelin-expressing ovarian cancer or cholangiocarcinoma, a cancer of the bile ducts. Twenty percent of patients who received gavo-cel experienced tumor shrinkage, and 13 percent had durable tumor regression.
“It was very exciting to see tumor shrinkage in some patients,” says Hassan, recalling one patient with mesothelioma who had already been treated with four previous therapies. “Just before this study she was thinking of going to hospice, but she had a pretty dramatic response to treatment with gavo-cel — almost a complete response that was maintained for about one year.”
Hassan notes that, while not all patients responded to the therapy and some had serious side effects, this study shows proof of principle that it is possible to target solid tumors using adoptive T-cell therapy. He and his colleagues will continue investigating novel T-cell therapies with the hope that even more patients will respond as these therapies evolve.