Anish Thomas, MBBS, M.D.
- Center for Cancer Research
- National Cancer Institute
- Building 10 Room 4-5330
- Bethesda, MD 20892
- 240-760-7343
- anish.thomas@nih.gov
RESEARCH SUMMARY
Small-cell lung cancer (SCLC) is the most fatal and highly metastatic form of lung cancer which kills at least 200,000 people globally each year, including approximately 30,000 individuals in the United States. Most patients with advanced SCLC die within a year of their diagnosis, and less than 5% of patients survive two years. My career commitment as a medical oncologist is to improve the lives of patients with SCLC through better understanding of SCLC. Starting in 2014, we have built a new clinical and translational research program for SCLC in CCR. Using SCLC as a paradigm of aggressive cancer, we aim to understand and eventually target (i) tumor plasticity and heterogeneity (ii) metastases and (iii) chemoresistance.
Areas of Expertise
Information for Patients
Learn more about our clinical trials and the highly specialized care teams that lead them.

Anish Thomas, MBBS, M.D.
Clinical Trials
Research
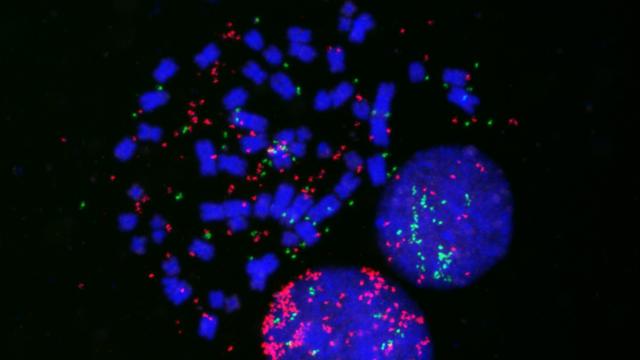
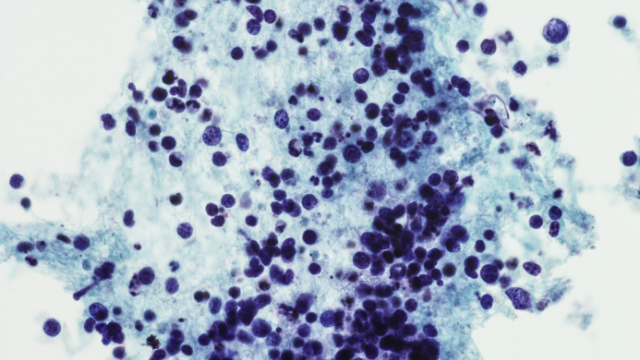
We apply a bed-to-bench-side approach to translational research (Cancer Cell 2022). Some of our key findings include: (i) Revealed replication stress as a transformative vulnerability of SCLCs characterized by high neuroendocrine differentiation (Cancer Cell 2021), (ii) Defined LMNA as a guardian of genome stability in SCLC (by maintaining FG-nucleoporin nuclear pore organization and RNA export; its loss causes RNA retention → R-loops and replication stress), a characteristic “indistinct nucleoli” morphology, heightened metastatic propensity, and determinant of response to replication-stress-targeted therapies (PNAS 2025), (iii) validated replication stress response mediator ataxia telangiectasia and Rad3 related as a tractable SCLC target (J Clin Oncol 2018), (iv) discovered of a novel SCLC subset defined by the germline genotype and improved responses to DNA repair targeted drugs (Sci Trans Med 2021), (v) Provided insights into the genomic and transcriptomic features that render low neuroendocrine SCLC more sensitive to immunotherapy (Nat Commun 2021), (vi) highlighted the transcriptional complexity of SCLC patient tumors in relation to patient-derived xenografts (Nat Commun 2022), (vii) and discovered extrachromosomal DNA (ecDNA) (Cancer Discovery, 2023) and tumor microenvironment (Cell Rep Med, 2024) as drivers of SCLC heterogeneity. We are actively investigating non-invasive methods to map SCLC heterogeneity – both genetic (Genome Med, 2025) and transcriptional (bioRxiv 2025) – using plasma-based approaches. Additionally, through the NCI rapid autopsy program, we are developing xenograft models (bioRxiv 2025) to better understand the organ-specific adaptations that drive SCLC metastasis.
To enable combinations of DNA-damaging therapy, we are investigating engineered drug carriers to extend circulation time, maximize intratumoral exposure, and mitigate dose-limiting toxicities. Strategies include PEGylation (Mol Cancer Res, 2022), liposomal (Oncologist, 2023), and nanoparticle (Nat Comm, 2025) delivery, HSP90-targeted miniature drug conjugates (ASCO, 2020), and antibody- drug conjugates (Clin Can Res, 2023).
Altogether, our studies have defined previously unrecognized therapeutic vulnerabilities and molecularly distinct SCLC subtypes, improving our understanding of this disease and our ability to care for patients with this disease. I am an elected member of the American Society for Clinical Investigation, and my work has been recognized by the NCI Director's Award for Clinical Science, NCI Director's Award for Translational Science, NIH Award of Merit, Federal Technology Transfer Award, and the PECASE Award, the highest honor bestowed by the U.S. government on outstanding scientists and engineers beginning their independent careers.
Since 2021, five of my trainees have received the American Society of Clinical Oncology (ASCO) Young Investigator Awards, which supports high quality research conducted by early-career investigators during their transition to a faculty appointment. Several post-doctoral trainee fellows currently hold physician-scientist or Assistant Professor positions in the US, Korea, Japan, France, and Hungary. My mentees have also been recognized by the International Association for the Study of Lung Cancer (IASLC) Early Career Award, NIH Fellows Awards for Research Excellence (FARE), NIH Physician-Scientist Early Investigator Award, Lasker Clinical Research Scholar Award, NCI Pathway to Independence Award for Outstanding Early Stage Postdoctoral Researchers (K99/R00), and have presented their findings at oral presentations at the World Conference on Lung Cancer (WCLC) and the American Association for Cancer Research (AACR) annual meetings. I was awarded the 2022 NCI Director’s Outstanding Mentor Award for exemplary mentoring and guidance of trainees and the 2024 NIH Postbac Distinguished Mentor of the Year Award. Since 2015, I have served as the Director of the NCI Medical Oncology Clinical Elective Program for medical students and residents.
Publications
- Bibliography Link
- View Dr. Thomas' PubMed Summary.
- View Dr. Thomas' ORCID page.
Metastatic Organotropism in Small Cell Lung Cancer.
Extrachromosomal DNA Amplification Contributes to Small Cell Lung Cancer Heterogeneity and Is Associated with Worse Outcomes.
Notch Signaling and Efficacy of Pd-1/Pd-L1 Blockade in Relapsed Small Cell Lung Cancer.
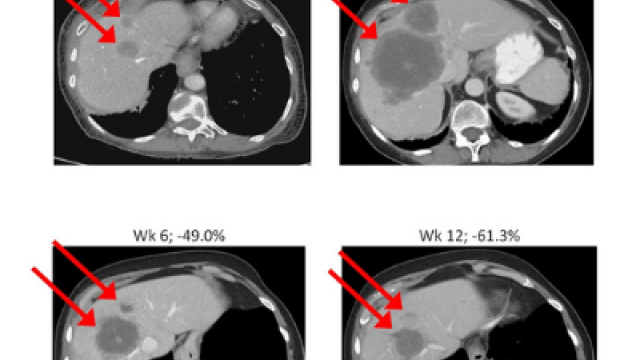
Therapeutic Targeting of Atr Yields Durable Regressions in Small Cell Lung Cancers with High Replication Stress.
Biography

Anish Thomas, MBBS, M.D.
Anish Thomas, M.D. is a medical oncologist who specializes in the treatment of thoracic cancers. He received his medical degree and postgraduate training in Internal Medicine from St. John's Medical College, Bangalore, India, following which he completed residency in Internal Medicine from State University of New York Upstate Medical University, Syracuse. He trained in Medical Oncology and Hematology at the Medical Oncology Branch of National Cancer Institute and the National Heart Lung and Blood Institute, respectively.
In 2023, Dr. Thomas received tenure at NIH.
Job Vacancies
We have no open positions in our group at this time, please check back later.
To see all available positions at CCR, take a look at our Careers page. You can also subscribe to receive CCR's latest job and training opportunities in your inbox.