Anish Thomas, M.B.B.S., M.D.
Anish Thomas, M.B.B.S., M.D., Lasker Clinical Research Scholar in the Developmental Therapeutics Branch, studies small cell lung cancer (SCLC). His goal is to develop more effective therapies for patients with SCLC and to better understand treatment response and resistance to improve the lives of people with this disease. In this Q&A, Dr. Thomas discusses the research questions he’s currently exploring and important research findings from his work studying SCLC.
What sparked your interest in lung cancer research?
I trained as a thoracic oncologist, and earlier in my career I worked on rare thoracic tumors, such as thymoma and mesothelioma. Prior to that, I trained and practiced as an internist in India. I became interested in small cell lung cancer around 2014 when I realized there was a need and an opportunity for more patient-driven research around this cancer.
SCLC is a highly aggressive cancer, probably one of the deadliest cancers, and the most lethal type of lung cancer. Most patients with SCLC die within a year of their diagnosis, and SCLC kills at least 200,000 people globally each year. Patients with SCLC derive little benefit from targeted therapies (treatments that use drugs to identify and attack specific types of cancer cells with less harm to normal cells) or immunotherapy, which is a type of cancer treatment that helps the immune system fight cancer. Despite the high toll on human lives, SCLC is treated largely using approaches developed over 30 to 40 years ago. My career commitment now is to advance the understanding of SCLC and treatment of patients with SCLC.
What are your current research interests? What questions or challenges are you currently pursuing?
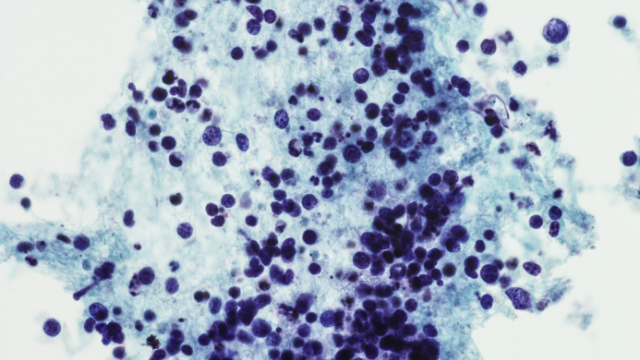
The overall goal of my program is to bridge the gap between the exponentially growing biological knowledge of cancer and its application to patients with SCLC, to hopefully improve their lives. We try our best to provide outstanding care for every patient and to learn from every patient, then apply what we’ve learned to the next patient. To this end, we leverage the dual powers of clinical observation and advanced genomic technologies and thoroughly study tumor biopsies from patients in relation to their clinical presentation, including family history, responses to treatment and more.
Understanding the basis of chemotherapy resistance and immunotherapy resistance are the two major challenges my lab is working on. Given that most patients with cancer – not just SCLC – die from treatment resistance, the drivers and determinants of this are important to understand. In clinical trials, we combine novel drugs with the goal of reversing chemo- and immunotherapy resistance.
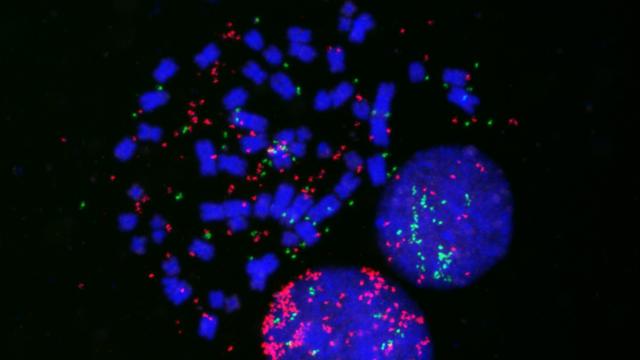
Another major challenge in the care of patients with SCLC is the lack of molecular subtypes that inform therapies. As a result, all patients are treated with the same therapies with a “one-size-fits-all” approach. We are working on identifying subgroups of SCLC that behave differently as well as the specific vulnerabilities of these subgroups. We're also trying to understand how tumor heterogeneity may be driving SCLC treatment resistance.
What important findings have you uncovered through this research?
In early-phase clinical trials we have identified a promising new combination therapy for patients with SCLC that comes back after initial treatment. The combination of berzosertib, a first-in-class drug that blocks a key DNA repair protein called ATR, and topotecan (a type of chemotherapy) is being tested in a couple of larger ongoing clinical trials. Successful clinical studies could lead to a new treatment paradigm for relapsed SCLC, an area of major unmet need, with only one drug approved in the last 25 years.
We have identified subtypes of SCLC with unique vulnerabilities. For example, a certain subtype of SCLC is more likely to respond to drugs that target the DNA replication process and another subtype more likely to benefit from immunotherapy. We've also found an SCLC subset driven by inherited mutations in DNA repair genes, challenging the long-held notion that SCLC is an exclusively tobacco-related cancer. Germline genotype (passed on from parents to offspring) could provide personalized treatment options for a small but important fraction of SCLC patients. Additionally, testing of family members of SCLC patients who harbor a cancer-predisposing germline mutation could potentially save thousands of lives through screening and preventive measures.
What are the future directions of your work?
Our ongoing studies aim to further subclassify SCLC into smaller groups, identify their unique vulnerabilities, and study the causes of heterogeneity.
How does the environment at CCR support your research?
My work would not have been possible outside of CCR. Specifically, the people, the scientific collaborations here, the environment that enables investigator-initiated clinical studies, the ability to focus on each patient, the ability to obtain research biopsies and follow patients on natural history studies, and the patients themselves and their caregivers who volunteer for the studies – many times out of purely an altruistic intent – all make the research possible.
What advice do you have for future generations of cancer researchers?
Although much has been accomplished in the field of cancer research, a lot of people still die from lung cancer. So, there is clearly a need and an opportunity to make a difference, especially in terms of applying the research advances to the care of patients with cancer.