A simple approach using viral peptides shows efficacy against diverse tumor types in mice.
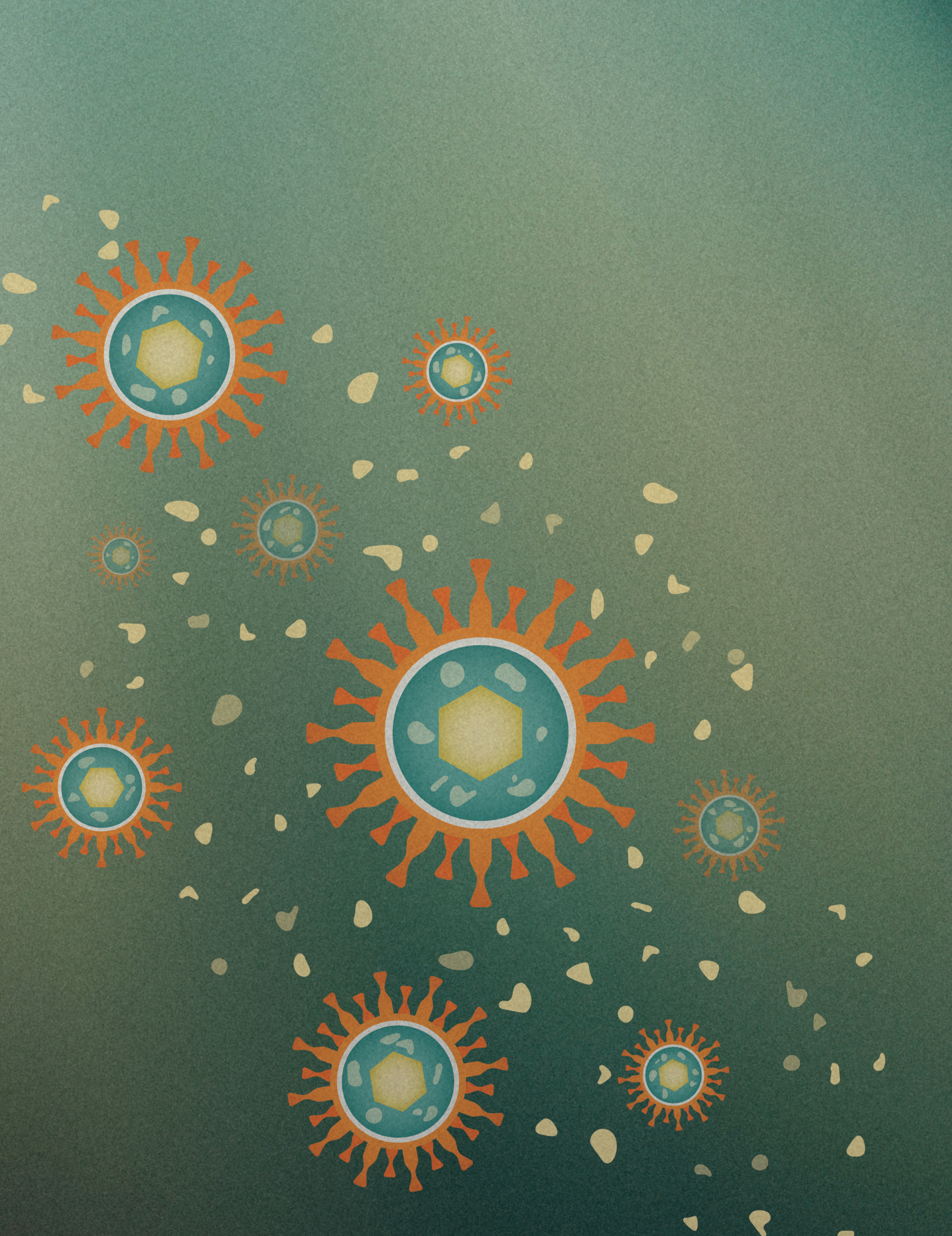
This diagram depicts cytomegalovirus (CMV), a common, usually harmless virus that has infected about 83% of humans around the world. By injecting pieces of proteins from CMV, shown here as pale yellow particles, directly into tumors, CCR researchers were able to activate preexisting anti-CMV T cells and reprogram the tumor microenvironment. This led to slower tumor growth and improved survival in mice with lung-, colon- and melanoma-derived tumors. Credit: Pamela Beltowski, SPGM, FNL, NCI, NIH
Many cancer therapies are becoming increasingly complex and reliant on expensive technologies, which threatens to exclude people in low-resource settings from access to effective treatments. To address this issue, Senior Investigator John Schiller, Ph.D., is searching for approaches that apply to a wider range of patients and that can be easily delivered, no matter where patients are located.
His idea is to harness existing long-term immunity that most people already have against common viruses. In an initial study, published in PNAS, Schiller and colleagues provide proof-of-principle for this approach using the cytomegalovirus (CMV), a common virus that has infected an estimated 83 percent of people around the world.
“The overwhelming trend in cancer therapy is to develop things that are highly personalized and complex, and if that trend continues there’s no way we’re going to reduce health disparities,” emphasizes Schiller. “So, we’ve been trying to develop de-personalized approaches that involve a simple intervention against a broad range of cancers at a relatively low cost.”
Through Schiller’s pioneering research on human papillomavirus (HPV) vaccines to prevent cervical cancer, it became clear that HPV virus-like particles can bind to and infect cancer cells but not healthy cells in intact tissues. This inspired Schiller and Staff Scientist Nicolas Çuburu, Ph.D., to explore using CMV to target cancer. The investigators speculated that infecting tumors with a few CMV genes would fool the immune system into thinking that the tumor cells are infected with CMV and eliminate them.
Initial experiments introducing CMV genes into the tumors of mice did not yield significant results. But injecting short pieces of viral proteins that could directly bind to the surface of the cancer cells worked like gangbusters, says Schiller.
In mice with lung-, colon- and melanoma-derived tumors, the injection of viral peptides induced a strong response from two powerful cancer-fighting immune cells: CD4+ and CD8+ T cells. As a result, tumor growth was reduced and survival improved, regardless of cancer type.
Importantly, the approach also yielded a long-term anti-tumor response. When the researchers transplanted additional tumors into the mice four months after the initial injection of CMV peptides, the mice still maintained their anti-tumor immunity.
Next, Schiller plans to partner with Senior Scientist Amy LeBlanc, D.V.M., to explore this novel strategy in dogs with naturally occurring cancers. Schiller says he’s excited for this next step, because it could help lay the foundation for the research to eventually be translated into humans.
“There’s no guarantee it’s going to work, but we believe it’s worth the effort because the potential for bending the curve of cancer in low-resource settings is a worthwhile goal to have, even if it’s difficult,” says Schiller.