A. Rouf Banday, Ph.D.
- Center for Cancer Research
- National Cancer Institute
- Building 37, RM 1066A
- Bethesda, MD 20892
- 240-551-4691
- 240-858-7515
- rouf.banday@nih.gov
RESEARCH SUMMARY
The overarching goal of Rouf Banday's research is to understand the genomic alterations that govern the development of bladder cancer and confer resistance to therapies. His laboratory uses multi-omics, and in vitro/in vivo functional genomics approaches to identify cancer dependencies, and biomarkers for response and survival in patients with cancer. Dr. Banday's studies have identified genetic and molecular mechanisms that regulate APOBEC-mediated mutagenesis, a major mutational process in bladder cancer.
Areas of Expertise
A. Rouf Banday, Ph.D.
Research
Bladder cancer is the 10th most common neoplasm worldwide for which treatment options remain limited both for muscle and non-muscle invasive disease. The central goal of our research is to elucidate mechanisms and map therapeutically actionable pathways underlying genetic and molecular alterations in bladder cancer. Specifically, our lab uses functional genomics and bioinformatics approaches to explore molecular mechanisms that drive and support tumor progression, weaken or inhibit tumor-immune surveillance, and impart resistance to therapies. Three areas of research focus are:
1) Mechanisms underlying genetic alterations in bladder cancer
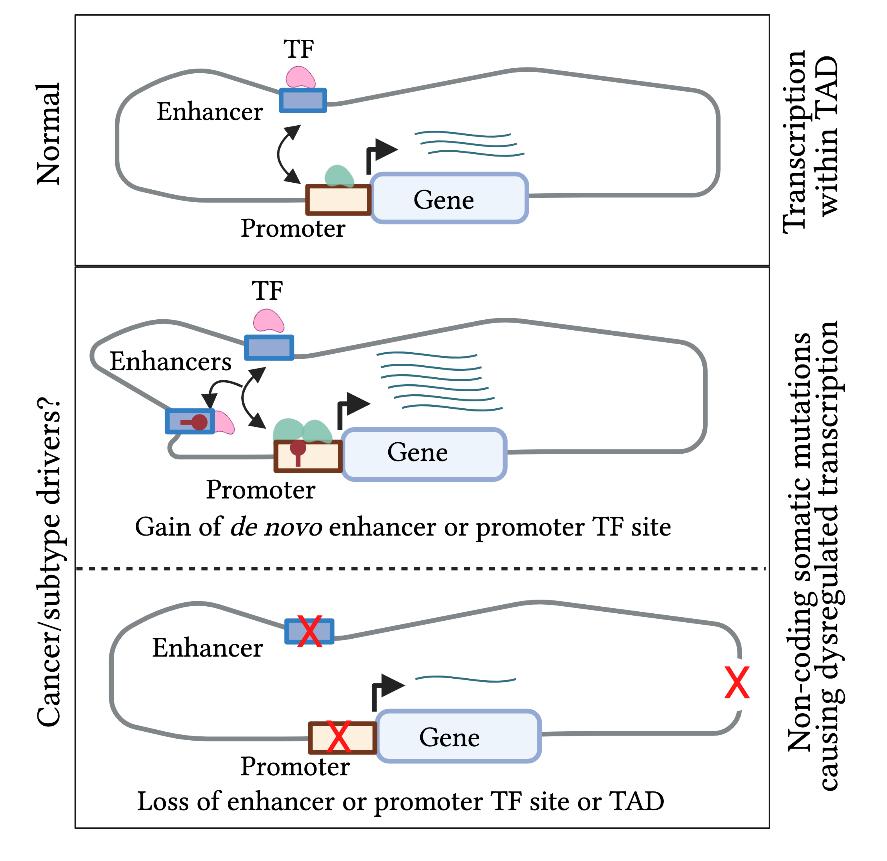
Mechanisms underlying genetic alterations observed in bladder cancer are largely unknown, particularly in the non-coding regions of the genome that can perturb gene expression through gain/loss of enhancer or promoter activity (Fig. A). We seek to a) identify functional non-coding genomic alterations and their target genes; b) explore their tumorigenic effects and interaction with coding driver mutations; and c) evaluate the effects of these alterations in modulating response to cancer therapies. Our lab uses tumor multi-omics data including from clinical trials, and CRISPR-mediated DNA editing, activation, and interference tools for massively parallel genetic manipulations in cells both in vitro and in vivo setting to characterize effects of genomic alterations on malignant cell transformation, tumor subtype speciation, epithelial-to-mesenchymal transition, metastasis, and interaction with therapies. Through these studies we aim to map bladder cancer dependencies that can guide design of novel drug targets and improve the utility of existing therapeutic agents.
2) Role of APOBEC3s in tumor evolution and interactions with cancer therapies
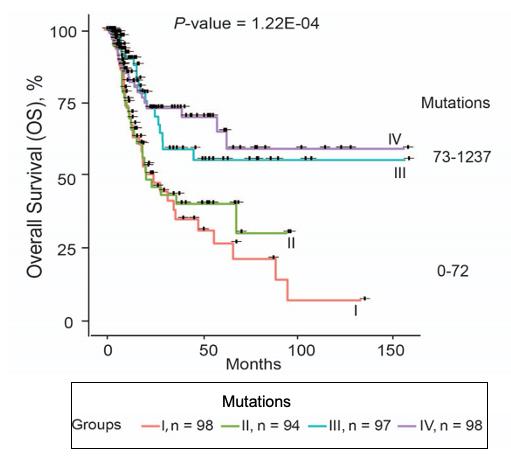
APOBEC3 enzymes, specifically APOBEC3A and APOBEC3B, have been implicated to play a central role in driving tumor evolution by causing somatic mutations commonly referred to as APOBEC-associated mutations/APOBEC-mutational signature. The spectrum of this mutational signature — both occurrence and total burden — vary within tumors of the same class and of different cancer types. These differences can indicate the intensity and duration of exposure to a specific mutagen, likely determined by cell-intrinsic regulatory mechanisms. For example, our studies have shown germline variants identified by GWAS increase expression of APOBEC3B and APOBEC3A/B deletion variant, leading to APOBEC-mediated mutagenesis and increasing cancer risk (Nat Genet 2016). But on the other hand, higher mutation burden in tumors can also improve patient survival potentially by increasing neoantigen repertoire (Fig. B). Additionally, alternative splicing of APOBEC3A and APOBEC3B could restrict APOBEC-mediated mutagenesis (Commun Biol 2021). In all, we have just begun to unravel the role of APOBEC3s in cancer biology, and studies in this field will greatly expand our understanding of tumorigenesis and how to use this information for therapeutic and preventive strategies. Our long-term goals are a) to explore how the biological and environmental triggers influence APOBEC3 enzymes to cause tumor mutations and drive tumor evolution; b) what cell/tissue-specific co-factors regulate these enzymes to prevent or promote their mutational activity; c) how these enzymes modulate immune infiltration and tumor microenvironment and affect the efficacy of cancer therapies; and d) ultimately, whether modulating expression of these enzymes improves or worsens clinical outcomes. My future studies will specifically focus on bladder cancer where APOBEC-induced mutations account for >67% of all single nucleotide somatic variation.
3) Explore and exploit RNA splicing dependencies in tumors as druggable targets for cancer therapy
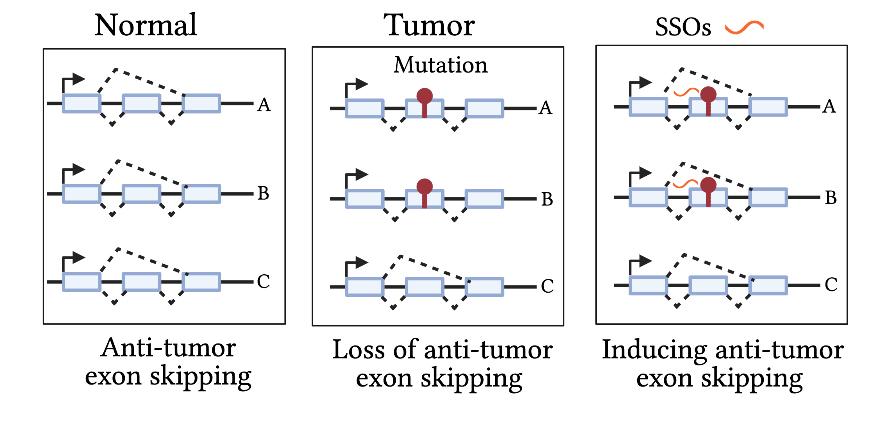
Tumors exhibit a high level of RNA splicing alterations driven by either direct mutations in splice cis-regulatory elements of genes including in tumor drivers or by mutations in trans-splicing factors SFRS2, SF3B1, U2AF1, RBM10, and ZRSR2. Mutations, including putative drivers, in these genes, are observed mutually exclusively in about ~ 15% of bladder tumors in TCGA (cbioportal.org). Conventionally, studies have focused on the role of aberrant splicing of single genes in cancer. High-throughput functional genomics approaches can be harnessed to systematically explore additive and synergistic effects of aberrant splicing modules in promoting carcinogenesis and resistance to therapies. We aim to explore data from large-scale bulk/single-cell RNA-seq projects, and lab-generated functional screens using CRISPR-mediated genome editing of splicing regulatory elements to identify splicing dependencies in tumors (Fig. C). Specifically, a) identify effects of recurrent intronic and synonymous mutations on splicing of tumor drivers; b) explore the role of mutated and dysregulated splicing factors such as SF3B1 in bladder tumorigenesis; and c) recreate systematically tumor-specific splicing dependencies and evaluate them for therapeutic purposes using nucleic acid-based strategies like antisense or splice switching oligos (SSOs).
Publications
APOBEC3-mediated mutagenesis in cancer: causes, clinical significance and therapeutic potential
Targeting natural splicing plasticity of APOBEC3B restricts its expression and mutagenic activity
Interferons and viruses induce a novel truncated ACE2 isoform and not the full-length SARS-CoV-2 receptor
Association of germline variants in the APOBEC3 region with cancer risk and enrichment with APOBEC-signature mutations in tumors
Biography
A. Rouf Banday, Ph.D.
Dr. Rouf Banday is a Stadtman Investigator in the Genitourinary Malignancies Branch at the Center for Cancer Research (CCR), National Cancer Institute. He received his B.Sc. from the University of Kashmir and completed both his M.Sc. and Ph.D. in biochemistry at Aligarh Muslim University, India. His doctoral research was supported by a prestigious Junior Research Fellowship from the Indian Council of Scientific and Industrial Research. During his Ph.D., he also received advanced training in bioinformatics at the University of Nottingham, UK, through a European Science Foundation fellowship.
Dr. Banday completed his postdoctoral training at the University of Connecticut and later joined the NCI’s Laboratory of Translational Genomics. His research has focused on bladder cancer genomics, uncovering key regulatory mechanisms of the APOBEC3A/B deaminases that drive tumor evolution. He also made notable contributions to innate immunity research, including the discovery of a novel interferon-inducible ACE2 isoform (dACE2) and investigations into genetic variation in OAS1.
His work has been recognized with numerous awards, including the AACR Scholar-in-Training Award, the NCI Director’s Innovation Award, FARE and DCEG-FARE awards, John Quale Travel Award from the Bladder Cancer Advocacy Network, Intramural Research Award, and the Milstein Award from the International Cytokine & Interferon Society.
Job Vacancies
We have no open positions in our group at this time, please check back later.
To see all available positions at CCR, take a look at our Careers page. You can also subscribe to receive CCR's latest job and training opportunities in your inbox.
Team
News
Learn more about CCR research advances, new discoveries and more
on our news section.