Clinical trials have traditionally been vital to advancing cancer prevention, diagnosis and treatment. Innovative new trial designs offer the opportunity to reach conclusive results faster, explore multiple treatment modalities and increase the diversity of patient cohorts towards developing treatments that benefit all patients.

Credit: iStock
Clinical trials have long been vital to advancing how we prevent, diagnose and treat cancer. Traditional clinical trials, however, can be cumbersome and slow. At CCR, we are enhancing the early development and clinical testing of new cancer therapies by closely integrating basic research with clinical science.
Traditional clinical trials consist of three phases. Phase I first-in-human trials establish a drug’s safety and determine the appropriate dose for subsequent testing by slowly increasing the dose administered. Phase II assesses a drug’s efficacy. If early trials succeed, an experimental treatment progresses to phase III where trials are randomized to investigate the treatment’s safety and efficacy compared to current standard of care. This process can take years and typically requires participation by hundreds or thousands of people.
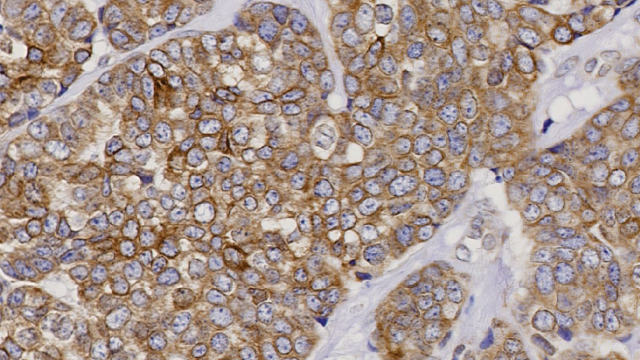
One major promise of new clinical trial approaches rests on the ability to identify patients more likely to benefit from a given therapy based on a detailed molecular profile of their tumor generated by genomic sequencing and molecular imaging. At a broader level, extensive genomic profiling of tumors is revealing that many common cancers can be classified into unique subtypes, which may respond to different drugs. This increased precision drives the need for more nimble and flexible trial designs that require fewer patients and can more rapidly determine a medication’s benefit.
Efforts are also underway to streamline and meld the three trial phases. Many new trials incorporate phase I/II designs in which an initial group of patients receives escalating doses of the drug until a safe dose is determined, and additional patients are then treated at this dose. Such approaches require fewer patients to evaluate a new treatment, reducing the time, cost and effort involved in recruiting study participants. This can be particularly valuable for trials of rare cancers that typically have a limited population from which they can recruit.
Today’s digital technologies, including molecular imaging, biometric sensors and health apps on smart phones, are revolutionizing the way cancer is diagnosed, treated and monitored. Credit: iStock
Today’s imaging and molecular analysis technologies have also created opportunities to enrich the data collected once clinical trials are underway. Molecular imaging and biometric sensors, as well as health apps on patients’ phones and mobile devices, allow researchers to obtain real-time, objective data to supplement information collected during intermittent clinic visits. Ultrasensitive methods can measure minute changes in tumor volume, for example, and phone apps can request daily input from a patient on levels of pain. Being able to aggregate and share the data generated by these clinical trial outcomes will be critical for facilitating the rational design of future clinical trials.
The ultimate goal of modern clinical trial design is to safely bring greater benefit more rapidly to more patients. We are implementing trial designs that allow as much learning as possible from small groups of patients, which is of critical importance when we test potential new treatments for rare cancers. Our priority is to make clinical studies as powerful and efficient as possible, to get new treatments to patients faster and to ensure they not only extend patients’ lives but improve them as well.