Prostate Cancer Genetics Section
Adam Sowalsky, Ph.D.
Research
Dr. Sowalsky's laboratory, the Prostate Cancer Genetics Section, conducts translational research focused on tumor evolution and treatment resistance, with a particular emphasis on developing biomarkers for predicting responses in locally-advanced prostate cancers treated by neoadjuvant hormonal therapies. By using samples from NCI clinical trials as human model systems for analysis, these correlative studies enable us to assess mechanisms of treatment resistance and develop strategies for precision therapy.
Current focus areas of research include: mechanisms of sensitivity to systemic neoadjuvant therapies in locally advanced prostate cancer prior to surgery, assessment of tumor evolution using circulating tumor DNA, and the interaction between tumor subpopulation diversity and treatment resistance.
Inquiries for postdoctoral training opportunities are always welcome.
Team
News
News from the Lab
Postbac Accepted into Medical School
June 25, 2025:
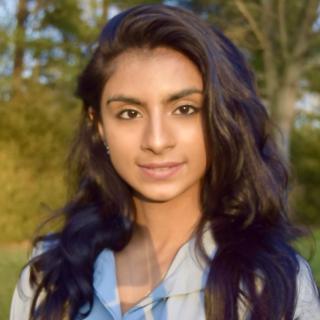
Congratulations to Sara Dawood for being accepted into Thomas F. Frist, Jr. College of Medicine!
Postbac Accepted into Graduate School
May 9, 2025:
Congratulations to Kayla Heyward for being accepted into Queen Mary University of London!
PCF YIA Grant Awarded to Postdoc
May 7, 2025:
Congratulations to Dr. Chennan Li for being awarded a prestigious Prostate Cancer Foundation Young Investigator Award.
Click here to read more...
DOD EIRA Grant Awarded to Postdoc
January 29, 2024:
Congratulations to Dr. Chennan Li for being awarded a prestigious Department of Defense Early Investigator Research Award.
Click here to read more...
Postbac Accepted into Graduate School
June 20, 2024:
Congratulations to Anna Baj for being accepted into Emory University!
Postbac Accepted into Medical School
June 12, 2024:
Congratulations to Daniel Low for being accepted into University of Washington School of Medicine!
Postbac Accepted into Medical School with Health Professions Scholarship
May 24, 2023:
Congratulations to Isaiah King for being accepted into University of Virginia School of Medicine with a Health Professions Scholarship from the United States Army!
Postdoc receives CCR Excellence in Postdoctoral Research Transition Award
November 30, 2021:
Congratulations to Dr. Scott Wilkinson for being awarded a CCR Excellence in Postdoctoral Research Transition Award.
PCF YIA Grant Awarded to Postdoc
November 10, 2021:
Congratulations to Dr. Anson Ku for being awarded a prestigious Prostate Cancer Foundation Young Investigator Award.
Click here to read more...
DOD EIRA Grant Awarded to Postdoc
October 29, 2021:
Congratulations to Dr. Anson Ku for being awarded a prestigious Department of Defense Early Investigator Research Award.
Click here to read more...
Postbacs Accepted into Medical School
June 30, 2021:
Congratulations to Nick Terrigino for being accepted into Lake Erie College of Osteopathic Medicine and to Jack Bright for being accepted into University of South Florida College of Medicine!
DOD EIRA Grant Awarded to Postdoc
April 2, 2019:
Congratulations to Dr. Scott Wilkinson for being awarded a prestigious Department of Defense Early Investigator Research Award.
PCF YIA Grant Awarded to Postdoc
November 18, 2018:
Congratulations to Dr. Scott Wilkinson for being awarded a prestigious Prostate Cancer Foundation Young Investigator Award.
Click here to read more...
Postbac Accepted into Medical School
November 15, 2018:
Congratulations to Nicole Carrabba for being accepted into McGovern Medical School!
Covers

A Subset of Localized Prostate Cancer Displays an Immunogenic Phenotype Associated with Losses of Key Tumor Suppressor Genes
Purpose: A subset of primary prostate cancer expresses programmed death-ligand 1 (PD-L1), but whether they have a unique tumor immune microenvironment or genomic features is unclear.
Experimental Design: We selected PD-L1–positive high-grade and/or high-risk primary prostate cancer, characterized tumor-infiltrating lymphocytes with multiplex immunofluorescence, and identified genomic alterations in immunogenic and nonimmunogenic tumor foci.
Results: One quarter of aggressive localized prostate cancer cases (29/115) had tumor PD-L1 expression more than 5%. This correlated with increased density of CD8+ T cells, a large fraction coexpressing PD-1, versus absent PD-1 expression on sparse CD8 T cells in unselected cases. Most CD8+PD-1+ cells did not express terminal exhaustion markers (TIM3 or LAG3), while a subset expressed TCF1. Consistent with these CD8+PD-1+TCF1+ cells being progenitors, they were found in antigen-presenting cell niches in close proximity to MHC-II+ cells. CD8 T-cell density in immunogenic prostate cancer and renal cell carcinoma (RCC) was nearly identical. Shallow RB1 and BRCA2 losses, and deep deletions of CHD1, were prevalent, the latter being strongly associated with a dendritic cell gene set in The Cancer Genome Atlas. Tumor mutation burden was variable; neither high microsatellite instability nor CDK12 alterations were present.
Conclusions: A subset of localized prostate cancer is immunogenic, manifested by PD-L1 expression and CD8+ T-cell content comparable with RCC. The CD8+ T cells include effector cells and exhausted progenitor cells, which may be expanded by immune checkpoint inhibitors (ICI). Genomic losses of RB1, BRCA2, and CHD1 may be drivers of this phenotype. These findings indicate that immunotherapies may be effective in biomarker-selected subpopulations of patients with localized prostate cancer.
Clin Cancer Res; 27(17); 4638–47, 2021.

Neoadjuvant-Intensive Androgen Deprivation Therapy Selects for Prostate Tumor Foci with Diverse Subclonal Oncogenic Alterations
Primary prostate cancer can have extensive microheterogeneity, but its contribution to the later emergence of metastatic castration-resistant prostate cancer (mCRPC) remains unclear. In this study, we microdissected residual prostate cancer foci in radical prostatectomies from 18 men treated with neoadjuvant-intensive androgen deprivation therapy (leuprolide, abiraterone acetate, and prednisone) and analyzed them for resistance mechanisms. Transcriptome profiling showed reduced but persistent androgen receptor (AR) activity in residual tumors, with no increase in neuroendocrine differentiation. Proliferation correlated negatively with AR activity but positively with decreased RB1 expression, and whole-exome sequencing (WES) further showed enrichment for RB1 genomic loss. In 15 cases where 2 or 3 tumor foci were microdissected, WES confirmed a common clonal origin but identified multiple oncogenic alterations unique to each focus. These findings show that subclones with oncogenic alterations found in mCRPC are present in primary prostate cancer and are selected for by neoadjuvant-intense androgen deprivation therapy. In particular, this study indicates that subclonal RB1 loss may be more common than previously appreciated in intermediate- to high-risk primary prostate cancer and may be an early event, independent of neuroendocrine differentiation, in the development of mCRPC. Comprehensive molecular analyses of primary prostate cancer may detect aggressive subclones and possibly inform adjuvant strategies to prevent recurrence.
Cancer Res; 78(16); 4716–30, 2018.
Lab Life
Mid-spring group picture (2025)
Back row (left to right): Ivy Yin, Adam Sowalsky, Anson Ku, Chennan Li, Nikhil Pramod, John Fenimore, Kayla Heyward
Front row: Sumeyra Kartal, Shana Trostel, Dava Vargas Solivan, Sara Dawood
Mid-summer group picture (2023)
Back row (left to right): John Fenimore, Chennan Li, Daniel Low, Scott Wilkinson, Adam Sowalsky
Front row: Sara Dawood, Anson Ku, Bella Silver, Shana Trostel
Seven members of the Sowalsky lab along with 4 members of the LGCP (plus 1 LGCP alumna!) go out to lunch in Denver, Colorado during the AACR Advances in Prostate Cancer Research conference (2023).
Beginning of summer group picture (2022)
Back row (left to right): Brian Capaldo, Isaiah King, Anson Ku, Scott Wilkinson, Adam Sowalsky
Front row: Shana Trostel, Melanie Sona, Nichelle Whitlock, Daniel Low, Anna Baj
Beginning of summer group picture (2021)
Back row (left to right): Adam Sowalsky, Jack Bright, Isaiah King, Brian Capaldo
Front row: Anson Ku, Shana Trostel, Nick Terrigino, Nichelle Whitlock
Head-on-a-stick: Scott Wilkinson
End of summer group picture (2019)
Back row (left to right): Scott Wilkinson, Jack Bright, Adam Sowalsky
Front row: Shana Trostel, Rayann Atway, Nick Terrigino, Nichelle Whitlock

End of summer group picture (2018)
Back row (left to right): Scott Wilkinson, Adam Sowalsky, Shana Trostel
Front row: Nichelle Whitlock, Tom Hennigan, Nick Terrigino, Nicole Carrabba
End of summer group picture (2017)
Back row (left to right): Adam Sowalsky, Rayann Atway, Nichelle Whitlock, Shana Trostel
Front row: Tom Hennigan, Scott Wilkinson

Friday afternoon get-together

A Christmas surprise for Scott

Showing off their matching T-shirts

End of summer group picture (2016)
Back row (left to right): Tom Hennigan, Adam Sowalsky, Shana Trostel
Front row: Beth Walton, Nichelle Whitlock
Head-on-a-stick: Scott Wilkinson