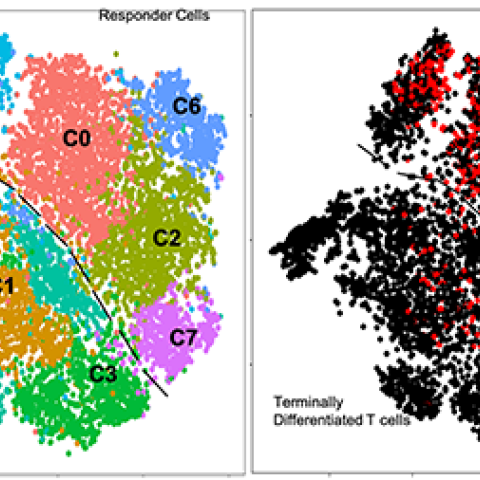
Analysis of over 20,000 individual T cells divide into separate clusters with different genetic markers and functional properties.
Image Source: Authors
CCR researchers used state-ot-the-art analytic techniques to determine characteristics of cells used in effective adoptive T cell therapy (ACT) in patients with advanced melanoma. Of the 56% of patients who experienced cancer regression, most had tumor infiltrating lymphocytes (TILs) lacking expression of CD39-CD69 markers, pointing to the importance of this feature in halting cancer growth. With knowledge of the characteristics of successful TILs, CCR researchers hope to apply this finding to immunotherapy for common cancers, including liver, breast, prostate, and colon cancer. These results appeared December 11, 2020, in Science.
Steven A. Rosenberg, M.D., Ph.D., Chief of the Surgery Branch, has been a leader in the field of immunotherapy, pioneering TIL therapy, which is a form of ACT. This approach uses T cells grown from the patients’ own tumors to produce large numbers of those T cells, which are then transferred back to the patients. “After 15 years of clinical trials in patients with metastatic melanoma, we now have data showing that about half of the patients have a good response, with about a quarter of that group having durable complete regression of cancer,” says Rosenberg. “What we didn’t know is why some patients respond so much better than others. This study has provided insight into key differences of the transferred lymphocytes.”
Sri Krishna, Ph.D., and Frank J. Lowery, Ph.D., postdoctoral research fellows in the labs of Rosenberg and Paul F. Robbins, Ph.D., Associate Scientist in the Surgery Branch, took the lead in this study. They explored the potential role of T cell differentiation state on patients’ responses to ACT by analyzing millions of T cells present in the administered infusion products using state-of-the-art single-cell genomic and proteomic analyses. From this extensive review, the team was able to identify the properties that led to tumor regression in patients who had undergone TIL immunotherapy treatment at the NIH Clinical Center. Grégoire Altan-Bonnet, Ph.D., Senior Investigator, Laboratory of Integrative Cancer Immunology, and his team, along with CCR’s Single Cell Analysis Facility at the NIH, contributed to this work.
“Through Krishna and Lowery’s work, we were able to identify surface characteristics of T cells that worked effectively,” says Rosenberg. “We determined that TIL negative for CD39 and CD69 had the self-renewing, stem-like characteristics crucial to success, while those that expressed CD39 and CD69 did not have these features, explaining the reason for different outcomes among patients. This discovery is the first human evidence identifying specific markers of adoptively transferred T cells that combat cancer successfully in humans.”
To further verify these findings, Rosenberg and his team transferred T cells with both CD39/CD69 negative and positive markers to mice harboring melanoma tumors. As they found in humans, the mice also showed tumor regression and higher survival rates when given self-renewing, tumor-specific T cells, those with negative CD39 and CD69.
Rosenberg anticipates manufacturing T cells with these characteristics to use in TIL therapy for melanoma. These results also have implications for immunotherapy for other kinds of cancer. Rosenberg is hopeful that this key information about which cells to use for transfer can be applied to treatment for other types of cancer.
“About 90% of all cancer deaths result from solid epithelial cancers such as colon, prostate, breast, and ovarian cancer,” notes Rosenberg. “To be able to unleash the most potent cells, those with stemlike characteristics, to patients with those kinds of cancer has the potential to save lives.”