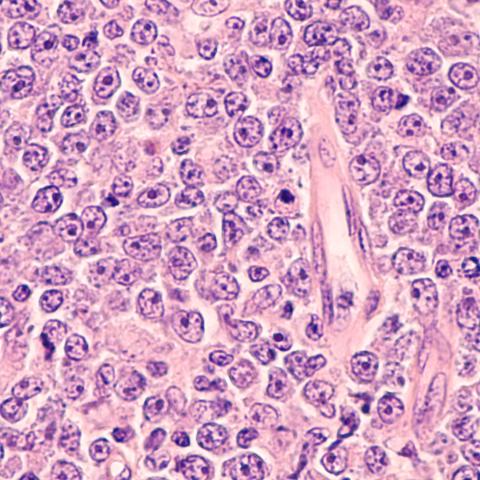
Photomicrograph of a diffuse large B-cell lymphoma (DLBCL). Image credit: rightdx/iStock
Innovative research has uncovered why some patients respond better to a tumor-killing treatment for diffuse large B-cell lymphoma (DLBCL) than others. The findings were reported in Cancer Discovery on April 25, 2024. Currently, 64.6% of people with DLBCL survive five years or more after diagnosis, but the new treatment has the promise to improve outcomes for some.
DLBCL is the most common type of aggressive non-Hodgkin lymphoma. Caused by an abnormal proliferation of white blood cells crucial to the immune system, DLBCL has typically been treated by chemotherapy regimens involving a combination of drugs. These drugs impact healthy and malignant cells alike, and many organs can be affected, so patients may experience many negative side effects. In response, researchers have devised an innovative strategy for a therapeutic treatment that targets only cancerous cells.
Louis M. Staudt, M.D., Ph.D., Chief of the Lymphoid Malignancies Branch, and his colleagues focused on cancer cells that were targeted by polatuzumab vedotin (Polivy), or "Pola-V” — the first new drug approved for DLBCL treatment in 20 years. They discovered patterns in clinical responses that indicate how Pola-V can be most effective in treating some diffuse large B-cell lymphomas.
“The biggest surprise was the role of sugars in regulating the cancer’s response to Pola-V,” Staudt said. “We showed that Pola-V, a monoclonal antibody drug linked to a chemotherapy drug, was dramatically hindered by sugars attached to its target, the B cell receptor.”
Based on this understanding of the attachment action of the sugar molecules, a process called glycosylation, the study looked to better clarify why some patients responded positively to Pola-V while some did not. This finding could be applied to improved treatment strategies for patients.
To confirm their observations, the researchers focused on the B-cell receptor CD79B, which is a glycoprotein on the surface of B cells. The receptor acts as a key regulator of the cell’s immune responses, signaling and functioning. Abnormal signaling can occur due to genetic mutations or other irregularities, which can result in uncontrolled cell growth that can become cancerous.
Using this receptor as a target, Pola-V binds with the CD79B marker, allowing for a robust immune response in compromised cells where a response might otherwise have been tamped down. The study determined that this approach benefited many patients, but in some, the CD79B receptor concealed itself. Here, complex sugar structures attached to CD79B could obscure the binding site, making it difficult for antibody molecules of Pola-V to find the cancer target.
These findings indicate a promising way forward for treating diffuse large B-cell lymphoma, one specifically tailored to patients most likely to respond to Pola-V while sparing them the side effects and toxicity of chemotherapy drugs. The researchers are also searching for ways to improve treatment for those with concealed CD79B receptors.
“Our findings suggest that inhibitors of glycosylation could be developed that would significantly boost the efficacy of Pola-V,” Staudt said. “There are a myriad number of enzymes responsible for glycosylation, suggesting that there may be numerous good opportunities for pharmaceutical development.”