Udo Rudloff, M.D., Ph.D.
- Center for Cancer Research
- National Cancer Institute
- Building 10 - Hatfield CRC, Room 4-3740
- Bethesda, MD 20892
- 240-760-6238
- 301-451-6933
- rudloffu@mail.nih.gov
RESEARCH SUMMARY
Dr. Rudloff’s laboratory and clinical work is focused on the discovery, translation, and early phase clinical testing of novel therapies for patients afflicted by pancreas and other solid organ cancers. His laboratory has built a program that discovers new leads for future cancer therapies from phenotype-directed drug screening. The best candidates with regard to (1) targeting essential cellular phenotypes of cancer, (2) chemotypes with favorable pharmaco- and toxicokinetic properties, and (3) a fully understood mechanism of action to facilitate future biomarker development and design of combination studies are selected as preclinical development candidates and moved into IND-enabling studies. His recent work includes the development and clinical translation of metarrestin, a small molecule for the treatment of cancer metastasis, which targets nucleolar genome organization of cancer cells, and a series of first-in-class small molecule-, peptide-, and nanobody-based innate defense modulators targeting CD206high tumor-associated macrophages for improved cancer immunotherapy.
Areas of Expertise
Information for Patients
Learn more about our clinical trials and the highly specialized care teams that lead them.

Udo Rudloff, M.D., Ph.D.
Clinical Trials
Research
Disease-focused Drug Discovery and Development in Pancreas Cancer
Current personnel, from left to right: Dandan Li, Biologist, Sitanshu Singh, Postdoctoral Fellow (Visiting), Soumita De, Postdoctoral Fellow (Visiting), Udo Rudloff, Head Translational Oncology Section POB, Saifun Nahar, Postdoctoral Fellow (Visiting), Rushikesh Sable, Research Fellow, Anju Kumari, Postdoctoral Fellow (Visiting)
Our laboratory aims to address the unmet medical need for more effective treatments of pancreas cancer patients. The overarching goal of the program is the development of novel therapeutics and therapeutic strategies to improve the life of pancreas cancer patients. Discoveries in the laboratory are tested in focused safety and proof-of-concept clinical trials, and observations made in the clinic are fed back to the laboratory to generate improved hypotheses and refine further preclinical research. Preclinical studies currently range from early structure-activity, in vitro, cell-based and in vivo evaluations, to PK, toxicokinetic, and IND enabling studies. Clinical protocols currently include the first-in-human protocol of metarrestin (ML-246) as a novel treatment for cancer metastasis. Many of these research efforts are conducted within a network of close collaborations which include medicinal chemists, biologists, pharmacologists, toxicologists, and regulatory experts from NCI, NCATS, Kansas University, and small pharma, whose expertise and contributions support further productive drug discovery and clinical translation.
I. Precision targeting of CD206high tumor associated macrophages
Rationale for tumor associated macrophages (TAMs) as a drug target
Cancer immunotherapy approaches in the form of immune checkpoint inhibitor or chimeric antigen receptor (CAR) T cell therapy have become first- or second-line treatment options in certain cancers, and in some patients confer sustained, durable treatment responses generally not observed with standard systemic chemotherapy. To-date, these positive findings are limited to immunologically ‘hot’ cancers. To the contrary, in the greater majority of solid organ cancers including pancreas cancer, which are classified as immunologically ‘cold’, the promise of immunotherapy via T cell activation has so far proven to be largely evasive. These tumors create an immune milieu which excludes cytotoxic T cells and/or induces ‘exhausted’ T cell phenotypes through an abundance of immune evasive cues frequently involving myeloid immune cells. Strategies that reinvigorate myeloid immune cells and convert cold tumors into immunologically hot, T cell-inflamed phenotypes would be a major advance in the field. Tumor associated macrophages frequently represent the largest fraction of myeloid cell infiltration in the tumor microenvironment (TME) of solid cancers. In the TME, TAMs exhibit a continuum of macrophage subsets with different functionalities and phenotypes ranging from ‘M1-like’ populations with proinflammatory, anti-tumor features to the CD163- and CD206-positive ‘M2-like’ immune suppressive, pro-tumor macrophage populations predominant in evolved cancers.
The mannose receptor 1 (Mrc1; CD206) is a bona fide innate immune checkpoint and immunotherapy drug target in oncology
Previous work by our group has identified the mannose receptor 1 (CD206) expressed on tumor associated macrophages (TAMs) as a novel stimulatory immune checkpoint and immuno-oncology target across different solid organ cancers. Activation of the CD206 receptor on CD206high TAMs reprograms and retools these cells hijacked by immune evasive cancer cells to mount effective innate and adaptive anti-tumor responses, sensitizes immune checkpoint inhibitor (ICI)-unresponsive tumors to PD-1/PD-L1 inhibition, and cooperates with standard-of-care therapies to improve tumor control.
A focus on small molecule drug development
The identification of CD206 as a novel innate immune checkpoint galvanized the development of a multidisciplinary, diverse drug development and translational research program by my group which has generated a comprehensive portfolio of small molecule-, therapeutic peptide, and nanobody-based CD206-targeting candidates with the goals of clinical translation and commercialization of the most promising candidate(s). In contrast to current primarily monoclonal antibody (mAb)-based immune checkpoint inhibitor (ICI) therapies, our program focuses on the development of small molecules to leverage improved tumor penetration and increased flexibility in difficult to perfuse cancers like pancreas cancer.
II. Preclinical and clinical development of metarrestin
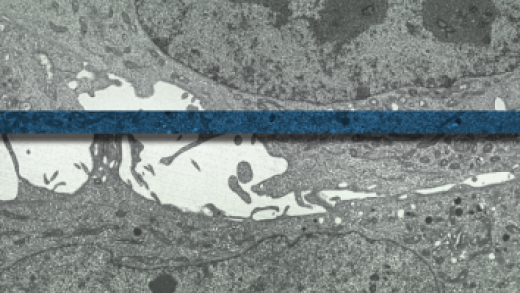
Metarrestin is a novel small molecular inhibitor with selective activity against the metastatic phenotype of cancer cells. Metarrestin targets a small nuclear structure, the peri-nucleolar compartment (PNC), and has impressive activity in pancreatic cancer metastasis models. Extensive pharmacokinetic studies have shown excellent tissue penetration of the drug with plasma : tumor AUC ratios exceeding 1 : 30 and intratumoral drug levels close to 100µM at non-toxic dose levels. Metarrestin is an oral treatment and is currently tested in a first-in-human clinical trial treating patients with advanced cancers. Metarrestin is well tolerated at dose levels reaching therapeutic levels in tumors. Despite preclinical toxicokinetic studies showing an increased risk of seizures and neurological side effects at high toxic dose levels in dogs, no serious side effects have been observed in patients treated with metarrestin at NIHs Clinical Center and the Kansas University Medical Research Institute. In the absence of dose limiting toxicities, dose escalation continues. Preclinical work conducted in parallel to clinical testing has identified a unique mechanism of action; metarrestin disrupts nucleolar ultrastructure and inhibits rDNA transcription which is informing break clinical biomarker development and future combination treatments.
Publications
- Bibliography Link
- View Dr. Rudloff's PubMed Summary.
Mannose receptor (CD206) activation in tumor-associated macrophages enhances adaptive and innate antitumor immune responses
The Changing Paradigm of Management of Liver Abscesses in Chronic Granulomatous Disease
Target Deconvolution of a Multikinase Inhibitor with Antimetastatic Properties Identifies TAOK3 as a Key Contributor to a Cancer Stem Cell-Like Phenotype
Merging perspectives: genotype-directed molecular therapy for hereditary diffuse gastric cancer (HDGC) and E-cadherin-EGFR crosstalk
Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for gastric cancer and other less common disease histologies: is it time?
Biography

Udo Rudloff, M.D., Ph.D.
Dr. Rudloff completed his M.D. at the University of Heidelberg, Germany. For his doctoral thesis at the German Cancer Research Institute, Heidelberg, he worked on gene regulation of rRNA transcription. He graduated from New York University in 2007 upon completion of his surgical residency training and pursued subspecialty training in surgical oncology by completing a 2-year surgical oncology fellowship at Memorial Sloan Kettering Center in New York City. Dr. Rudloff joined the NCI in July 2009 as an investigator and surgical oncologist. He is a physician scientist with a combined laboratory and clinical research effort focused on the discovery of novel cancer treatments and their development towards early phase clinical testing. Dr. Rudloff has been the recipient of several awards including the GFM Young Talent Price, ASCO Young Investigator Award, and NCI & NIH Director Awards of Merit for his translational science efforts. He successfully competed for support of IND-enabling studies of first-in-class cancer therapeutics developed by his group. He was awarded tenure by NIH in 2020.
Job Vacancies
We have no open positions in our group at this time, please check back later.
To see all available positions at CCR, take a look at our Careers page. You can also subscribe to receive CCR's latest job and training opportunities in your inbox.