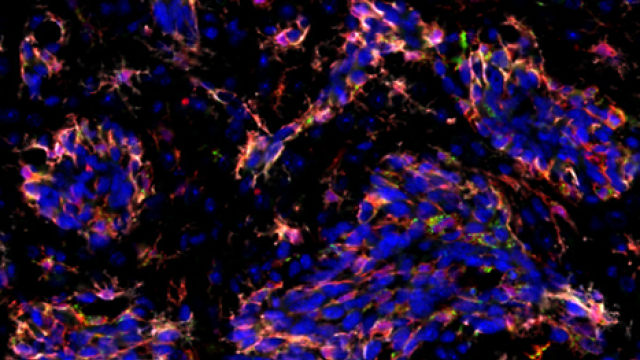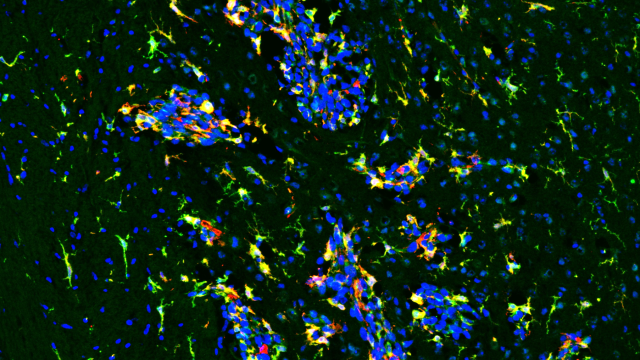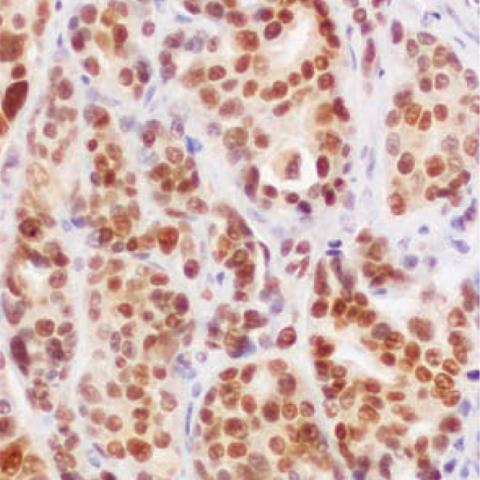
Immunohistochemical staining of a human brain metastasis.
Image credit: Patricia S. Steeg, Ph.D.
In a phase I clinical trial of a drug combination that aims to prevent metastatic tumors from recurring in the brains of women with advanced breast cancer, 83 percent of patients developed no new brain metastases. Trial participants, who had HER2-positive breast cancer and had previously been treated with radiation or surgery to eliminate metastatic tumors in the brain, received a combination of low-dose temozolomide (TMZ) and T-DM1. Results of the phase I study, which included 12 participants who were followed for three to 34 months, appeared January 27, 2023 in Clinical Cancer Research.
The trial, led by Alexandra Zimmer, M.D., a former CCR associate research physician who is now an associate professor at Oregon Health and Science University, builds on work by Patricia Steeg, Ph.D., Deputy Director and Senior Investigator in the Women’s Malignancies Branch. Steeg’s work showed that TMZ prevents breast cancer from metastasizing to the brain in mice.
More than a third of women diagnosed with advanced cases of HER2-positive or triple-negative breast cancer eventually develop metastatic tumors in the brain. The metastases are often treated with radiation or surgery, but new lesions usually develop soon. The incidence of such metastases has risen as modern treatments have enabled women with advanced breast cancer to live longer. This is in part because many of the therapies used to stop the spread of the disease have difficulty getting to the brain: a protective blood-brain barrier keeps most drugs out.
TMZ, a chemotherapy drug that is used as a first-line treatment for an aggressive brain cancer known as glioblastoma multiforme, can efficiently cross the barrier to enter the brain. While TMZ does not appear to shrink metastatic breast cancer tumors once they have established themselves in the brain, Steeg and her colleagues discovered that in mice, a low daily dose of the drug can prevent these tumors from forming. “It's not that we reduced brain metastases; we didn't get any over a 10-fold span of doses,” Steeg says. “I've never seen anything like it.”
For the first clinical test of TMZ as a potential prevention for breast cancer brain metastases, Steeg, Zimmer, and their colleagues focused on a particularly high-risk group: women who had already developed and been treated for metastatic lesions in the brain. All entered the trial within six weeks of their last surgery or radiation treatment. While none of the participants had detectable new tumors at the start of the trial, Steeg’s lab’s analyses of cerebrospinal fluid collected at that time indicate that six of the 12 participants did have cancer-associated DNA present in their brains. That suggests cancer cells were present in the brain and these patients had a very high risk of getting new tumors.
Patients in the study received TMZ daily at one of three doses, along with T-DM1, a drug that is commonly used to treat HER2-positive breast cancer. All experimental TMZ doses were low compared to the dose of TMZ that is used in a treatment setting. Participants were followed for an average of 9.6 months. The drug combination was well tolerated and only two patients developed new tumors in their brain tissue.
More than four years after the trial’s launch, one participant remains on the experimental drug regimen, with no new tumors. The team is now exploring a possible phase I clinical trial to evaluate a drug combination that includes TMZ as a prevention for secondary breast cancer metastasis in women with triple-negative breast cancer.