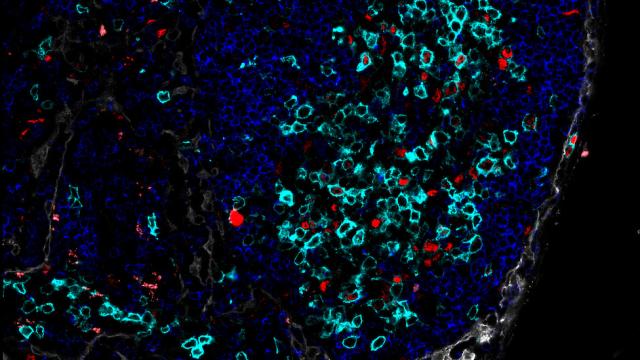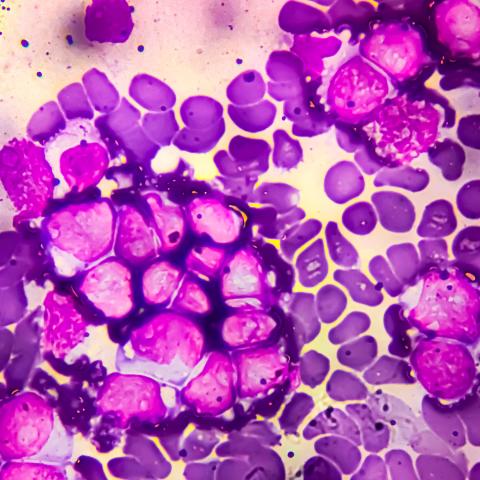
Microscopy image of B-cell acute lymphoblastic leukemia. Credit: iStock
New research has shed light on why a specialized form of cancer therapy that targets the immune system, called CD22 CAR T-cells, works in some patients but not others. The study, led by Nirali N. Shah, M.D., Lasker Clinical Research Scholar in the Pediatric Oncology Branch, was published March 13, 2025, in Molecular Therapy.
Chimeric antigen receptor (CAR) T-cell therapy is a treatment in which T cells, a type of immune response cell, are harvested from patients and genetically modified in a lab to attack targets on the surface of cancer cells. These modified cells are reinfused into a patient’s body to attack the cancer. In this study, researchers looked at CD22 CAR T-cell therapy, in which the T cells were programmed to target the CD22 receptor molecule on the surface of cancer cells. CD22 CAR T-cell therapy was first developed in the Pediatric Oncology Branch and received breakthrough therapy designation by the U.S. Food and Drug Administration (FDA) in 2019.
Previously, a phase 1 trial conducted by Shah’s team evaluated samples from 54 patients and found that CD22 CAR T-cell therapy had a 70% response rate, which is an impressive result for an early-phase trial. But the goal of this project was to learn about what happens when the CAR T cells don’t work, said first author Alexandra Dreyzin, M.D., a Staff Clinician in the Center for Cellular Engineering at the NIH Clinical Center.
In this study, the researchers analyzed samples of cells extracted from patients, the starting materials for CAR T-cell manufacturing, and the modified cells that were to be reinfused into the patient. The cells were from pediatric and young adult patients with a blood cancer known as relapsed or refractory B-cell acute lymphoblastic leukemia and who had been treated with CD22 CAR T cells.
Notably, there were no significant differences in baseline disease characteristics or demographic factors between patients who responded to treatment and those who did not. Instead, the difference seemed to lie in the condition of the patients’ immune cells. Specifically, some patients had T cells that showed signs of exhaustion and differentiation, which seemed to indicate that these immune cells were at a later stage of development.
“There are markers on the surface of cells and genetic markers that we can look at to tell us where in the life cycle T cells are. What we have learned is that CAR T cells that are more likely to be effective tend to be in an earlier stage of development, more activated, and without these markers of exhaustion on them,” said Dreyzin.
The researchers also noticed that the difference in T cells existed at baseline at the start of the study and after the genetic modification process.
“What we could see is that the cells that comprised the starting material from patients’ cancers that did not respond to CD22 CAR T cells were already more differentiated than the cells in the starting material from patients who did well,” Dreyzin said. “As the cells went through modifications, that difference got more pronounced, but it was there at the beginning.”
Two potential questions for future research include: what caused the difference in the T cells, and how the modification cycle affects T cells, as the process can be stressful for the cells and can accelerate differentiation that is already present. Changes to the modification process of the T cells that are reinfused into a patient could not only reduce the stress to cells, but even potentially improve outcomes for patients who are starting with unfavorable cells.
“This CAR-T cell therapy has really transformed the field in terms of how effective it can be, and Dr. Dreyzin’s research and contributions on our team help take us to that next step, to understand how we can make it even more effective,” said Shah.