Patricia S. Steeg, Ph.D.
- Center for Cancer Research
- National Cancer Institute
- Building 37, Room 1-126
- Bethesda, MD 20892
- 240-760-6828
- 301-675-4647
- steegp@mail.nih.gov
RESEARCH SUMMARY
Dr. Steeg investigated mechanisms of breast cancer metastasis. She discovered the first metastasis suppressor gene, nm23 (NME). Her recent work investigated brain metastasis of breast cancer. The Steeg lab identified pathways that mediate brain metastasis, potential preventives, and studied the composition and role of the blood-tumor barrier. An open Phase I/II clinical trial of low dose, metronomic temozolomide for secondary prevention of brain metastases of breast cancer is based on the lab's preclinical data.
Areas of Expertise
Research
Molecular Characterization of Breast Cancer Metastasis to the Brain/Central Nervous System.
The Steeg lab mechanistically investigated breast cancer metastasis to identify and preclinically credential new preventives and therapies. Tumor metastasis, the movement of tumor cells to new sites in the body and their progressive colonization, is a major contributor to patient morbidity and mortality. While clinical trials are regularly conducted in the metastatic setting, few drugs have been approved that actually target mechanisms of metastasis.
The major focus of the lab was on the brain and central nervous system (CNS) lesions. Additional projects in the lab included breast cancer in young patients and the Nm23/NME metastasis suppressor gene.
Brain metastases develop primarily in metastatic patients with HER2+ tumors, often in the setting of responding or stable systemic disease, and in triple-negative (estrogen and progesterone receptors negative, HER2 normal, TN) tumors in the setting of uncontrolled systemic disease. Brain metastases are thought to be increasing in incidence as systemic therapy improves, more imaging is performed, and drugs continue to be excluded from the brain. The impact of brain metastases on patients is devastating in terms of physical consequences and neurocognitive declines, resulting from both the lesions and their treatments.
Secondary Prevention of Brain Metastases of Breast Cancer. Preclinical research in the Steeg lab credentialed low-dose, metronomic temozolomide (TMZ), a brain permeable therapeutic, as an effective preventive for brain metastases of breast cancer (Clin. Cancer Res, 20: 2727-2739, 2014). Briefly, TMZ effectively prevented the formation of brain metastases in mice over a several-log dose range, and extended survival, including “cures”; TMZ had no activity against established, large brain metastases in keeping with the clinical literature. Screening of human brain metastasis craniotomy specimens showed that HER2+ brain lesions expressed the lowest levels of known resistance mechanisms.
Dr. Alexandra Zimmer, Women’s Malignancies Branch, CCR completed a phase I “secondary prevention” trial (NCT03190967) of low dose, metronomic TMZ in HER2+ patients. The trial enrolled patients with HER2+ breast cancer and previously treated brain metastases to T-DM1 as systemic therapy and increasing doses of TMZ. A manuscript is in preparation. A phase II trial is in the planning stage, as is a phase I/II trial for TN disease. The primary endpoint is novel, freedom from a new brain metastasis over a predetermined period of time. The Steeg lab worked with Dr. Zimmer on exploratory endpoints including sequencing of cell-free tumor DNA (cfDNA) in CSF and serum (with DNAseq on the primary tumor block); potential molecular correlates of neuroinflammation and neuronal viability; potential CNS-derived exosome number and content in serum; MGMT status; patient-reported outcomes.
Characterization of the Blood-tumor barrier (BTB). The blood-brain barrier (BBB) is an intricate cellular/matrix encasement of brain capillaries, designed to regulate substance entry and thereby preserve brain metabolism. When a metastasis forms, the BBB is termed a BTB, but its architecture and functionality are poorly understood. The Steeg lab collaborated with CNS pharmacologists to show in multiple preclinical mouse models that the permeability of the BTB to drugs or markers is heterogeneous and that only a small fraction of metastases had sufficient permeability to permit a cytotoxic response to chemotherapy. A presurgical study of neurosurgical patients provided confirmation of heterogeneous drug uptake.
Based on these data, the lab hypothesized that: (a) the BTB is not a chaotic breakdown of the BBB, but a series of consistent alterations; (b) that the transition from a low- to a higher permeability BTB in brain metastases also occurs by consistent alterations; (c) that these same alterations are found in human brain metastases and; (d) that one or more alterations functionally modulates permeability of the BTB. Major efforts on this project included:
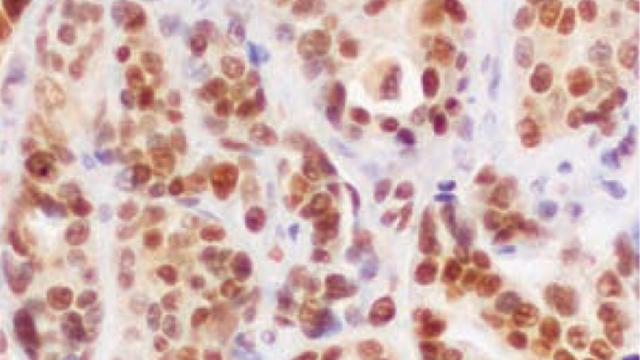
- Comparison of the BBB vs. BTB and low- vs. high permeability BTBs for conventional CNS proteins in three model systems. Multiple, consistent alterations were found when a BBB became a BTB. With altered permeability of the BTB, fewer consistent changes were found, notably a correlation of higher permeability and a subpopulation of desmin+ pericytes (Clin. Cancer Res. 22: 5287-5299, 2016)
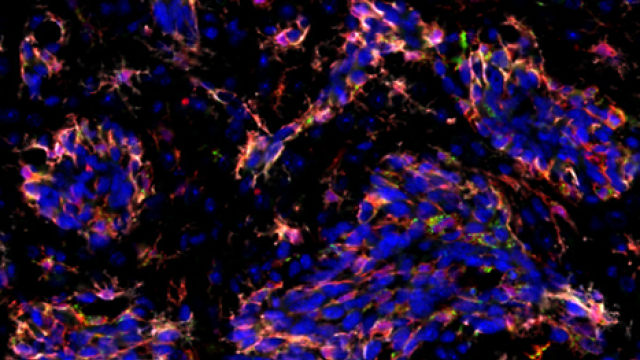
- An agnostic gene expression analysis was performed on low- and higher permeability brain metastases from the same mouse brain, identifying new molecular correlates of permeability. Expression of the sphingosine-1 phosphate receptor 3 (S1P3) was higher in neuroinflammatory astrocytes in higher permeability metastases in four model systems. Antagonists to S1P3 tightened the BTB in vivo. Using a “Trojan horse” approach, tumor cells expressing S1P3 trafficked this signaling behind the BTB and increased lesion permeability in vivo (Nature Comm. 9:2705, 2018).
- The permeability of the BTB toward larger monoclonal antibody therapeutics was probed using two brain tropic model systems and an experimental biparatropic antibody-drug conjugate (ADC) to HER2. ADC uptake in brain metastases was heterogeneous but provided some metastasis preventive activity. Interestingly, ADC uptake was not correlated with traditional markers of paracellular BTB permeability and in vitro data suggested a transcytosis mechanism (Neuro-Oncology. 22:1625-1636, 2020).
Leptomeningeal Metastasis (LM) of Breast Cancer. The Steeg lab developed mouse models of LM metastasis to provide additional mechanistic and translational insights. The project was supported by a DOD Breast Cancer Research Program Breakthrough grant W81XWH1810737.
Breast Cancer in Young Patients. Numerous epidemiological studies demonstrate that patients, when diagnosed with breast cancer at a young age (typically <40), have a poor outcome. Many factors correlate with young age including African-American race, triple-negative and luminal subtypes, large tumors or poor grade, early metastasis, etc., but multivariate analyses consistently demonstrate that, after these variables are accounted for, young age at diagnosis portends a poor outcome. Studies of primary breast tumors fail to find many genetic or molecular alterations that may be responsible. In collaboration with the lab of Dr. Lalage Wakefield, CCR, the Steeg lab hypothesized that a young host may cause increased tumor aggressiveness (Clin. Cancer Res. 27:4422-4434, 2021). Metastasis in TN and luminal B mouse model systems was used as a readout of aggressiveness. Key findings include:
- When tumor cells were inoculated into young and older mice side-by-side, no differences in lung or liver metastases were detected. In contrast, young mice developed ~3-fold greater brain metastases than older mice.
- Immune components of the brain change with age. A decline in microglia and potentially infiltrating macrophages was observed. Depletion of these populations with a colony-stimulating factor 1 receptor (CSF-1R) inhibitor significantly prevented brain metastases, preferentially in young mice.
The data identify a host pathway causative for increased brain metastases in young animals and support the hypothesis that age-specific mechanistic pathways and therapies can be identified.
NME/Nm23 Metastasis Suppression. I discovered the first metastasis suppressor gene, nm23 (nme). Over- or re-expression of metastasis suppressor genes into metastatic tumor cells significantly reduced metastasis with no effect on primary tumor size. The field now includes >30 genes that shed light on metastatic pathways distinct from primary tumor growth. I investigated mechanisms of action and sought means to bring metastasis suppression to patients. Nm23 function in suppression of breast cancer motility in vitro was dependent on the tumor cell endocytic process and uncovered an Nm23-Dynamin2 (DNM2) interaction leading to DNM2 oligomerization and activation (Cancer Res. 79:4689-4702, 2019).
Publications
- Bibliography Link
- View Dr. Steeg's PubMed Summary
Biography

Patricia S. Steeg, Ph.D.
Dr. Patricia S. Steeg received her Ph.D. from the University of Maryland in 1982 and was a Jane Coffin Child Memorial Fund for Medical Research Fellow in the Laboratory of Developmental Biology and Anomalies, National Institute of Dental Research, and the Laboratory of Pathology, NCI, where she was tenured in 1992. She became the Deputy Chief of the Women's Malignancies Branch, CCR, NCI in 2014. Dr. Steeg was also the Co-Director of the Office of Translational Resources, CCR, NCI.
Dr. Steeg retired from CCR as the Deputy Chief of the Women's Malignancies Branch in February 2025 and is now an NIH Scientist Emeritus.