Cancer researchers have identified an effective treatment in mouse models for targeting gliomas carrying genetic abnormalities known as IDH mutations.
By Raleigh McElvery, Scientific Communications Editor
February 27, 2023
Over the past decade, researchers have been working to understand how an alteration in genetic code known as an IDH mutation causes certain cancers. The isocitrate dehydrogenase (IDH) enzyme regulates many life-sustaining chemical reactions within a cell, and changes to its DNA can trigger cells to multiply uncontrollably. This can result in several different types of cancers including glioma—a cancer of the brain and spinal cord that’s especially difficult to treat.
Now, in a new study published in Clinical Cancer Research, a team of researchers from the NCI Center for Cancer Research’s Neuro-Oncology Branch (NOB) and the NIH’s National Institute of Neurological Disorders and Stroke led by Chunzhang (Spring) Yang, Ph.D., has pinpointed the molecular events that allow IDH-mutated glioma cells to continue to spread. Based on these findings, the scientists identified a drug called ipatasertib that works in combination with the common chemotherapy temozolomide (TMZ) to slow tumor growth and prolong survival in preclinical mouse models. The researchers hope these findings will help develop more effective cancer therapies with better outcomes for people with IDH-mutated gliomas.
“Cancers with certain genetic backgrounds often develop vulnerabilities, and when we find these weak points we can transform them into actionable targets to treat the disease,” says Dr. Yang, who heads the NOB’s Molecular and Cell Biology Research Program. “Curative therapy is currently unavailable for IDH-mutated gliomas, but this study and others are pioneering innovative treatments with the potential to improve patient outcomes.”
IDH mutations are quite common in gliomas; in fact, over 80 percent of grade 2 and 3 gliomas contain these genetic changes. While patients with these tumors generally live longer, there is still an urgent need to develop more effective treatments for the disease. And, in some cases, those with lower-grade IDH-mutated gliomas are more likely to experience a recurrence and progression to a higher grade.
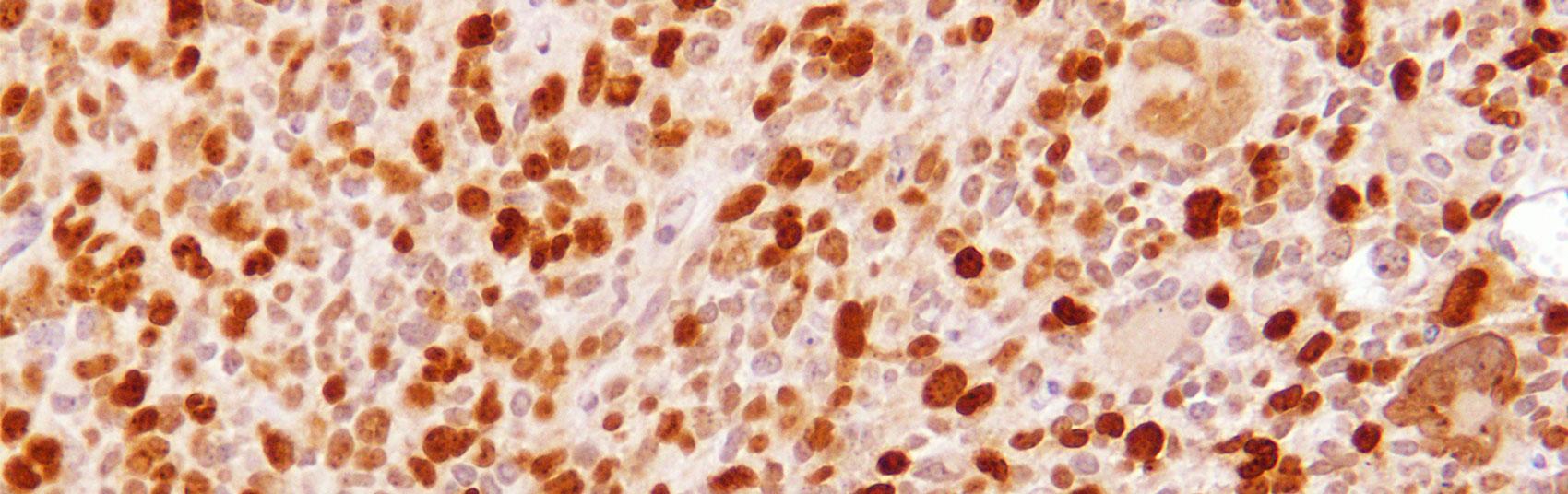
Several years ago, Dr. Yang’s lab was combing through a rich database of genomic data called The Cancer Genome Atlas. They noticed a peculiar pattern: Although tissue samples from glioma patients with and without IDH mutations appeared nearly identical under a microscope, upon closer inspection their patterns of gene expression were quite different. Since this discovery, Dr. Yang has been working to understand precisely why these changes in gene expression can cause IDH-mutated gliomas to spread and resist treatment.
Scientists have known for many years that mutations in the IDH enzyme impact a cell’s metabolism in ways that would kill any normal cell. However, in their new study, Dr. Yang’s team found that IDH-mutated glioma cells develop a workaround to thrive despite this metabolic stress. The researchers determined that these cells protect themselves by activating a cascade of molecular events known as the AKT/Nrf2 pathway. This ultimately increases the expression of certain genes, allowing the cells to not only evade death but also continue to multiply and form tumors.
To prevent IDH-mutant cells from activating this protective AKT/Nrf2 pathway, Dr. Yang and his collaborators tested several different drugs that target an important protein in the pathway called protein kinase B (often abbreviated PKB or AKT). Of all the experimental drugs the researchers tested in their mouse models, ipatasertib was the most effective. It also made the IDH-mutated glioma cells more sensitive to the chemotherapy TMZ.
Although there are several ongoing clinical studies testing ipatasertib on solid tumors—including metastatic breast cancer, head and neck cancer, non-small cell lung cancer, and even a type of glioma known as glioblastoma—Dr. Yang says there are very limited studies assessing its efficacy in patients with IDH-mutated gliomas specifically. “Our work in animal models is a strong justification for the next step, which would be an early-phase clinical trial,” he explains.
In the meantime, Dr. Yang’s team is continuing to probe the molecular underpinnings of glioma development and progression. Given that there are multiple subsets of gliomas with varying genetics, he emphasizes that there likely won’t be a one-size-fits-all treatment.
“I think the take-home message of this study is that IDH-mutated gliomas have a distinct genetic background, so designing specific therapies based on their unique biological pattern will be the most effective approach and have the greatest benefit for the patient,” he says.
Top image caption: Microscopy image of glioma cells from the researchers’ preclinical mouse model. Credit: Dr. Yang