As head of the Molecular and Cell Biology Program, Dr. Chunzhang Yang investigates whether genetic mutations in cancer cells could serve as therapeutic targets.
By Raleigh McElvery, Scientific Communications Editor, Neuro-Oncology Branch
August 11, 2022
Researchers recently uncovered a mystifying paradox: The very genetic mutation that spurs some cells to become cancerous also renders them especially sensitive to treatment. As the head of the Neuro-Oncology Branch (NOB) Molecular and Cell Biology Research Program, Chunzhang (Spring) Yang, Ph.D., is on a mission to understand this biological contradiction—and harness it to devise more effective cancer therapies.
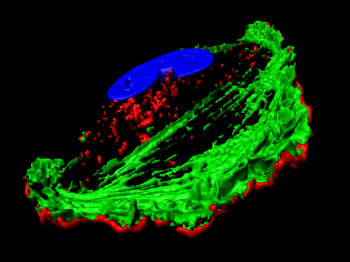
Dr. Yang’s team focuses on glioma, the most common type of malignant primary brain tumor in adults. Over 80 percent of lower-grade gliomas have a mutation in their genetic code that affects an enzyme known as isocitrate dehydrogenase (IDH). IDH is critical for cell metabolism, but mutations can trigger it to take on new biological functions that transform the cell from healthy to cancerous.
Because this genetic change incites tumor development, it’s somewhat counterintuitive that patients with IDH-mutated gliomas often exhibit a better prognosis and live longer than patients with other tumor types. To Dr. Yang and others, this signals that—despite driving cells to become cancerous—IDH mutations also establish weaknesses that ultimately make tumors more responsive to treatment.
“We view the IDH mutation as a vulnerability in the cancer cell,” Dr. Yang explains. “Our goal is to better understand this vulnerability and to exploit it as an opportunity for therapeutic intervention, developing experimental therapeutics that improve the current standard of care for patients.”
Prior to arriving at the NOB, Dr. Yang earned a bachelor’s in medicine and a Ph.D. in neurobiology from Peking University in China. He then moved to the United States to complete his postdoc at the National Institute of Neurological Disorders and Stroke. Around this time, one of his family members was diagnosed with a brain tumor, motivating him to dedicate his career to probing fundamental questions about central nervous system cancers. In December of 2015, he packed up his office and moved across the NIH’s Bethesda campus to begin his stead at the NOB’s Molecular and Cell Biology Program.
Getting to Know the Enemy
Although brain tumors are among the deadliest of diseases, Dr. Yang explains that the therapies to treat them have remained relatively unchanged since the early 2000s.
“We’ve learned a lot about brain tumor genetics and biology in the past two decades,” he says, “but there’s been limited improvement in disease outcomes. To better our current approaches, we need to get to know our enemy in the most fundamental sense. What drives these tumors? What are their therapeutic vulnerabilities? Most importantly, we need to understand each tumor’s unique biology, because every one is different.”
Physicians have three primary lines of defense against brain tumors: surgery, chemotherapy, and radiation. The latter two approaches work by damaging the cancer cells’ DNA in an attempt to suppress the malignancy. However, cancer cells have advanced resistance mechanisms to repair their broken DNA and continue to manifest.
IDH-mutated gliomas, however, appear to have an Achilles' heel: They’re less adept at mending their DNA, and so Dr. Yang is experimenting with various drug compounds that could further cripple these tumors’ repair response. The drug candidate he is most interested in is called a PARP inhibitor, and it has already been approved by the FDA to treat BRCA-mutated breast cancers.
In addition to PARP inhibitors, Dr. Yang has also been investigating another class of compounds called Nrf2 inhibitors. Nrf2 inhibitors prevent cancer cells from maintaining the metabolic balance they need to counteract the buildup of toxic chemicals that naturally occurs when a cell contains an IDH mutation. By starving the cell of antioxidants, Nrf2 inhibitors induce such intense metabolic stress that the cell dies.
Using this information, Dr. Yang’s ultimate goal is to develop a therapeutic regimen that targets multiple molecular pathways in IDH-mutated gliomas—for example, combining a PARP or Nrf2 inhibitor with chemotherapy. “A full dose of one drug alone may only have limited efficacy, but combining several compounds may result in drug synergy and stronger efficacy, which helps curb tumor growth while reducing side effects for the patient,” he explains.
Collaborating Beyond the Lab Bench
Outside the lab, Dr. Yang spearheads several efforts to bring established researchers from around the country to the NOB, facilitating innovative research partnerships and educational opportunities. He co-chairs the NOB’s Visiting Scholars Program, and also organizes workshops introducing early-career trainees to established neuro-oncologists.
His favorite part about being a member of the NOB is the collaborative atmosphere and free exchange of ideas.
“Here, we’re really on a fast track to clinical translation,” he says. “While my team is hard at work at the lab bench, our colleagues are interfacing with real patients to help us understand and perform disease-relevant experiments. It’s a powerful system that ultimately provides the basis for improving patient care.”