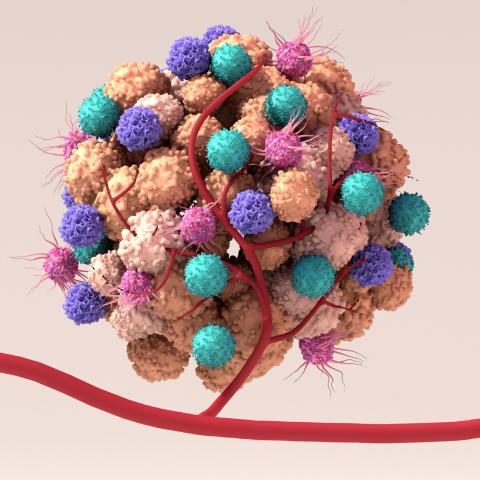
Artist depiction of a tumor microenvironment, including normal, immune, and cancer cells as well as blood vessels that surround and feed the tumor cells. The microenvironment can affect how a tumor grows, spreads and responds to treatment.
Credit: Design Cells, iStock
CCR researchers created one of the largest collections of RNA expression and immune profile data for pediatric cancers to date, revealing a common protein target for novel treatment approaches. The researchers, as part of a collaborative effort led by Javed Khan, M.D., Deputy Chief of the Genetics Branch, analyzed 788 extracranial solid tumors and cancer cell lines from 14 different types of pediatric cancer. From this work, the researchers identified several targets for immune therapy and validated a potential multi-pediatric cancer target — a germline and tumor-specific protein called PRAME. Their work, published in Cell Reports Nov. 23, 2021, provides a way forward to better target and treat currently incurable pediatric cancers.
Pediatric solid tumors that spread beyond their site of origin are notoriously difficult to treat. “It’s devastating because once pediatric cancer has spread, there’s no cure in a majority of cases,” Khan says. To find the best way to treat these pediatric cancers, Khan and his colleagues took a multipronged approach. They established cancer-specific immune signatures and used RNA expression profiles to find common targets for immunotherapy.
The team found that tumors with more immune cell infiltration signified a better prognosis for the patient, especially for osteosarcoma, a type of bone cancer. “This indicates that there is immune activity happening in these tumors,” Khan explains. But they also found that some pediatric cancers have a combination of cell surface proteins (called immune checkpoints) that might bolster immune system evasion, which has implications for the efficacy of therapy selection for each cancer type.
One type of therapy that Khan hopes to explore for pediatric solid tumors is adoptive T-cell therapy. During this type of therapy, a patient’s own T cells are extracted and engineered in the lab to target cancer-specific proteins, leading to T cells that attack only cancer once the T cells are reinjected in the patient. To identify proteins to target, Khan’s team compared gene expression profiles between tumors and healthy tissue samples. They found that many pediatric cancer types express the protein PRAME, making it a potential multi-pediatric cancer target.
In a proof of principle experiment, Khan and his colleagues exposed osteosarcoma and Ewing sarcoma cell lines to T cells engineered to recognize PRAME. In both cases, the specialized T cells attacked the cancer cells but not the control cells. Subsequently, the team showed that the engineered T cells decreased tumor amounts in a mouse model of aggressive Ewing sarcoma.
The investigators’ next step will be to develop these findings into therapeutic applications. “The time is right because T cell-engineering is much easier than it used to be, and we can test this approach in animal models very quickly,” Khan says. “It’s not a slam dunk — there’s a lot of work to be done. But this is the way forward for potentially treating pediatric solid tumors in a precise and potent manner, and which may be less toxic than chemotherapy.”