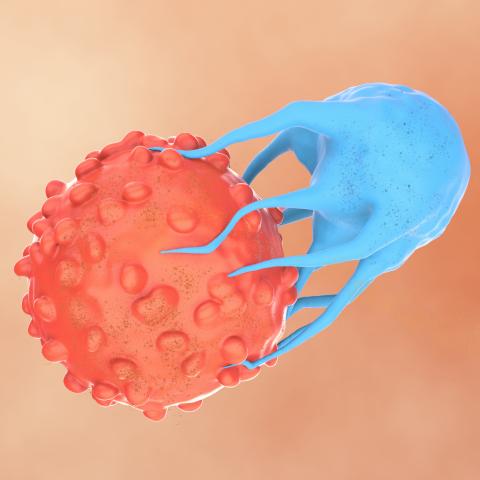
Illustration depicting a CAR T cell (blue) attacking a cancer cell (orange). Image: iStock
Research from CCR scientists points toward a strategy for making chimeric antigen receptor (CAR) T-cell therapy, the cell-based immunotherapy that has revolutionized the treatment of some blood cancers, safer and more effective for treating solid tumors.
The study, led by Grégoire Altan-Bonnet, Ph.D., Deputy Chief of the Laboratory of Integrative Cancer Immunology, Naomi Taylor, M.D., Ph.D., Senior Investigator in the Pediatric Oncology Branch, and Paul François, Ph.D., at the University of Montréal, shows how adding certain receptors to CAR T cells can prevent the cells from attacking healthy tissue while simultaneously enhancing their activity against cancer cells. The findings appeared April 10, 2025, in Cell.
CAR T-cell therapy reprograms patients’ immune cells to be effective cancer killers using genetically engineered chimeric antigen receptors (CARs) that are added to their T cells. CARs are designed to recognize molecules on the surface of cancer cells called antigens, which can usually be found on some healthy cells, too. This leads to manageable side effects for patients with blood cancer, but when CAR T cells designed to target solid tumors attack healthy tissue, the effects can be severe.
T cells, the immune cells used in CAR T-cell therapy, can also recognize cancer cells using T-cell receptors (TCR). TCRs trigger a weaker immune response than CARs, but they adeptly discriminate between cancer cells and healthy tissue. So Taylor, Altan-Bonnet and their colleagues explored the impact of adding both types of cancer-targeting receptors to the same T cell.
Postdoctoral researcher Taisuke Kondo, D.V.M, Ph.D., and graduate students Sooraj Achar and François Bourassa led the effort to test T cells featuring both TCRs and CARs. They found that while strong activation of a TCR could amplify an immune response, weakly activated TCRs could reduce T cells’ response to their CAR targets. Multiple parameters, including the quality and concentration of antigens, influence a TCR’s activation in response to any given cell.
The finding was surprising, but the researchers realized that if they selected the right TCR to pair with a CAR, they could achieve two desirable effects: boosting a T cell’s response against cancer cells through strong TCR activation and reining in the cell’s response against healthy tissue through weak TCR activation.
The cross-talk between TCRs and CARs is complex, so the researchers developed a machine learning program to predict the behavior of T cells with combinations of receptors. They used this model to create CAR T cells with a built-in braking system to protect healthy tissue. They selected a TCR that would be strongly activated by mutated antigens on the cancer cells, amplifying the T cells’ response against their intended targets. In contrast, when these T cells encountered the non-mutant antigen on healthy cells, it would only weakly activate the TCR, keeping T-cell activity in check, even in the presence of the CAR-activating antigen.
The group engineered mice that produced both healthy and cancerous human tissues so they could test their dual-receptor T cells. The results demonstrated clear benefits to their approach. T cells with just a TCR did a poor job of controlling tumors cells. Cells with just a CAR destroyed healthy lung tissue. But when the same CAR and TCR were combined, the T cells eliminated tumor cells and left healthy tissue intact.
With the group’s mathematical model, researchers can now explore how other TCRs might be added to CAR T cells to promote strong anti-cancer responses that leave healthy cells undisturbed — potentially overcoming one of the biggest obstacles to CAR T-cell therapy for solid tumors.


