Alison (right) with her husband, Don. Credit: Alison James
Alison James is a small business owner and mother from Texas. She has an active lifestyle, and until recently, was very healthy. “In May 2024, I woke up one morning and I had a knot on the side of my neck about the size of a pecan,” she said. “I hadn’t really had any issues like this before, so this was kind of a left turn for me.”
Doctors at her regional hospital diagnosed Alison with squamous cell carcinoma in her tonsils and three lymph nodes. Squamous cells make up the lining of internal organs and are the most common cell type affected by HPV-associated cancers. The positive news for Alison was that her prognosis was very good — squamous cell carcinoma of the oropharynx (tonsils and base of tongue) is highly curable. However, the standard of care for this diagnosis typically involves radiation therapy to the neck, which can majorly impact quality of life.
“Of all the treatments that we use for head and neck cancer, radiation is the one that can have the most long-term side effects,” said Clint T. Allen, M.D., Senior Investigator in the Surgical Oncology Program. This treatment method can cause dental issues, fibrosis, or stiffening, of the muscles in the mouth and throat, and toxicity to the salivary glands, resulting in problems with swallowing, speaking and salivating.
Alison wasn’t satisfied with this option, so her doctors in Texas helped her seek alternatives. This led her halfway across the country to the NIH Clinical Center where Dr. Allen leads a clinical trial testing an alternative treatment regimen for HPV-associated cancers of the oropharynx.
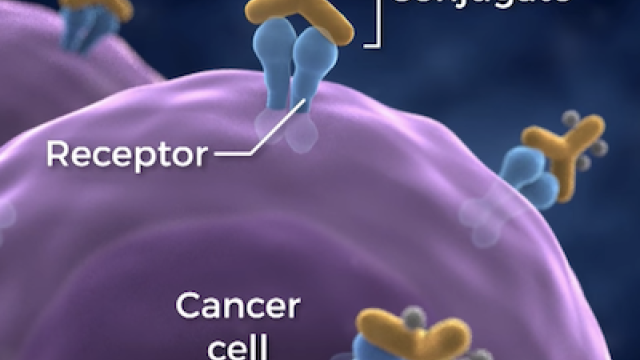
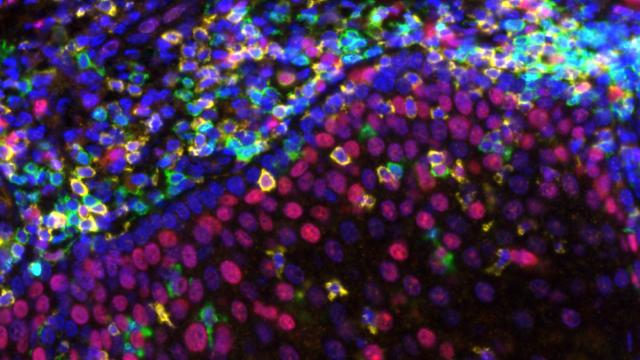
Typically, patients with Alison’s diagnosis receive either chemotherapy and radiation or surgery, which may still be followed by chemotherapy and radiation depending on what is found in the biopsy. Other physicians have noticed that chemotherapy before surgery can lead to pathology reports that show no features that indicate a need for radiation after surgery, Dr. Allen explained. Based on such observations, his clinical trial uses a combination of two chemotherapy drugs and surgery to treat the cancer and minimize the chances of needing radiation after the surgery. Half of the patients are also randomly assigned to receive an immunotherapy treatment to create a stronger anti-tumor immune response. If the results show positive outcomes, this trial could be an important first step in reducing the use of radiation for all patients with HPV-associated cancers of the oropharynx.
Charalampos Floudas, M.D., D.M.Sc., M.S., Associate Research Physician in the Center for Immuno-Oncology and medical oncologist for this clinical trial, explains that CCR is uniquely positioned for this kind of early-stage trial. “The Clinical Center is an independent and nonbiased institution that often conducts trials that aim to change the standard of care,” he said. “Also, this research requires significant laboratory research expertise and that's something that we have here.”
Alison was excited for the opportunity to participate and receive treatment that reduced the possibility that she would need radiation. “I felt like if I could avoid all of these side effects, I needed to take that chance,” she said. After screening, she was accepted into the clinical trial and assigned to the group receiving the additional immunotherapy. That meant traveling to the NIH Clinical Center seven times over two months for all of her treatments.
The treatments and travel paid off. After the chemotherapy and immunotherapy, Alison received positive news from her surgeon. “I had my left tonsil and 22 lymph nodes in my neck removed, and the pathology results showed no cancer,” she said. “It was completely obliterated by the chemo.”
Dr. Allen and Dr. Floudas were also pleased with this result. If they continue seeing positive outcomes, they are hopeful for a larger, multi-center clinical trial to further validate their results and continue the path to expanding the standard of care for this cancer to include neoadjuvant, or pre-surgery, chemotherapy with or without immunotherapy to reduce reliance on radiation.
Alison has her own hopes for the future. Her youngest son is about to start college, and the family is planning a trip to Italy this summer. “I’m able to enjoy all of these experiences because I had this opportunity,” she said. Alison credits the team in CCR for treatment that was not life-changing, but “life-sustaining,” allowing her to keep living her normal life without the major side effects.