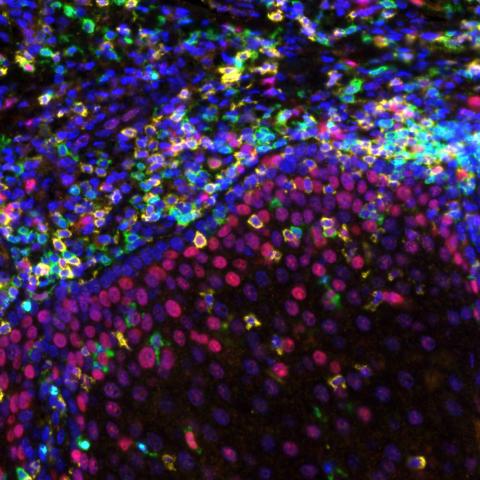
Immunofluorescence image shows CD4+ (green) and CD8+ (yellow) T cells in the microenvironment of a head and neck squamous cell carcinoma.
Credit: Allen Lab.
New evidence uncovered by CCR researchers may explain why treating head and neck cancers with the immunotherapy checkpoint inhibitor drug bintrafusp alfa before surgery may be more effective at preventing disease recurrence than surgery alone. The results, which show that bintrafusp alfa increases the number and spread of tumor-fighting immune cells throughout a patient’s body, were published April 13 in Cancer Cell.
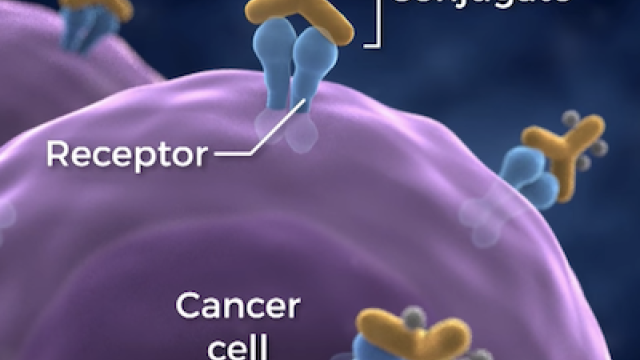
T cells are a type of immune cell responsible for attacking and killing cancer cells. But when T cells have been exposed to cancer for long periods of time, they can become covered in proteins that interfere with their ability to fight cancer and are called exhausted T cells. Immune checkpoint inhibitors are a class of drugs that help revitalize exhausted T cells in the fight against cancer.
Patients with head and neck cancers unrelated to human papillomavirus (HPV) typically do not receive treatment before surgery to remove the tumors, but recent evidence suggests that treatment with an immune checkpoint inhibitor before surgery can decrease the chances of the cancer recurring afterwards. Clint T. Allen, M.D., Senior Investigator in the Surgical Oncology Program (SOP), and his team decided to conduct a study to better understand the molecular underpinnings of this phenomenon.
The researchers took blood and tumor samples from six patients with head and neck squamous cell carcinoma (HNSCC) unrelated to HPV, both before and after the cancers were treated with bintrafusp alfa. They performed single-cell analyses of individual T cells from the tumors before and after treatment and paired these results with analysis of T cells in the blood.
The results showed that, before treatment with bintrafusp alfa, exhausted T cells were almost exclusively found in tumors. But after treatment, these exhausted T cells gained a renewed ability to attack cancer cells and were more abundant in both tumors and circulating in patients’ blood. “We think this is a very significant finding and may help to explain why these therapies work so well at decreasing the risk of disease recurrence,” explains Allen.
By increasing the number of tumor-fighting T cells throughout a person’s body before surgery, bintrafusp alfa may help prevent cancer from recurring or spreading after the procedure.
Cem Sievers, Ph.D., is a computational biologist in the SOP who performed the computational analyses for the study. Another important finding, he notes, is that evidence of elevated glutamine metabolism appears to identify T cells that respond poorly to the treatment. Glutamine is an amino acid that T cells can use for sustenance under certain environmental conditions. “This could potentially be important — it means that if we alter glutamine metabolism while delivering the drug, this could further enhance T-cell activity and patients’ response to the therapy,” he explains.
Together, these results may lead to more effective treatment strategies to prevent HNSCC from recurring after surgery.