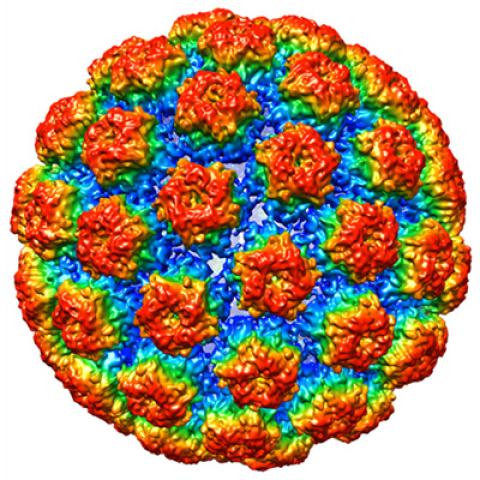
The structure of HPV 16, which causes cervical cancer.
Photo courtesy of Christopher Buck
A phase I/II clinical trial at the NIH Clinical Center will test the effectiveness of a vaccine against cancers linked to the human papillomavirus (HPV). The vaccine will be tested alone and in combination with a checkpoint inhibitor called M7824. The phase I portion of the trial is currently recruiting between 12 and 18 people with advanced HPV-related cancer. They will be treated over a three-to-six-month period. Additionally, the phase II portion, which will be starting shortly, will focus specifically on people with localized head and neck cancer. They will be given the same treatment regimen as those in the phase I portion of the trial.
The vaccine is similar to adenovirus vaccines, which have been studied extensively and are known to be safe. An adenovirus can cause many common infections, including the common cold, sore throats and bronchitis.
Julius Strauss, M.D., Assistant Research Physician in the Laboratory of Tumor Immunology and Biology, is leading the study. He points out that while the field is moving toward studying earlier-stage HPV-linked cancers, he was interested in working to improve outcomes for those with more advanced disease.
“We’re hoping to see a partial or total remission over the course of the clinical trial,” says Strauss. “Patients with localized tumors, like those being recruited for the phase II portion of the clinical trial, have a 29 percent recurrence rate over a three-to-four-year period. Our goal is to extend the time before the cancer recurs.”
Strauss joins a long list of CCR researchers who have studied HPV-linked disease and have made breakthroughs in the field. Ten years ago, two CCR researchers, Doug Lowy, M.D., and John Schiller, Ph.D., both of the Laboratory of Cellular Oncology, performed the groundbreaking research that resulted in the HPV preventive vaccine. At the beginning of their work, they were aware that using any form of the HPV oncogene as a vaccine could cause the patient to be infected, but they discovered a potent alternative. The researchers found that multiple copies of HPV could re-assemble into virus-like particles, which galvanized antibodies to resist infection to HPV and prevent the development of cancers of the cervix, vulva, vagina, penis, anus and oropharynx (the area encompassing the back of the throat, the base of the tongue, and tonsils).
Although the preventive vaccine that eventually was developed based on Lowy and Schiller’s work, referred to as Gardasil, has been a game-changer, HPV-linked cancers have not been eradicated. According to NCI’s SEER database, between 2012 and 2016, 34,800 people were diagnosed with HPV-associated cancers, the two most prevalent being cervical and oropharyngeal cancer.
Christian S. Hinrichs, M.D., Senior Investigator in the Genitourinary Malignancies Branch, is working to add to the arsenal of potential treatments for HPV-associated cancer. Like Strauss, his research concentrates on late-stage cancers. The patients referred to his program have metastatic disease and are considered incurable. Hinrichs has been able to help many of these patients with his innovative approach, which uses genetically engineered T cells to shrink or eliminate tumors.
“Most scientists are familiar with CAR-T therapy, which uses chimeric antigen receptors to target antigens on the cell’s surface for hematologic malignancies,” explains Hinrichs. “But we can’t do that for HPV-associated cancers because there are no good targets on the cell’s surface. Instead, we use T cells that can target the viral antigens inside the cells that cause cancer. We have had some success with this approach.”
Hinrichs recently reported on the outcomes of a phase I trial using T-cell therapy in 12 patients who had previously been treated with a range of three to seven anticancer treatments. Six patients responded favorably with some tumors shrinking and others going away completely. The beneficial effects of treatment lasted between three to nine months. This trial is now in phase II and is looking to enroll as many as 40 more patients.
In a recently opened trial using T-cell therapy, Hinrichs began investigating a group of patients with advanced, but not metastatic, head and neck cancer. Typically, these patients are treated with a combination of chemotherapy and radiation. While this approach is effective, the side effects can be devastating. “We see patients who have experienced tightness and pain in the skin, loss of saliva, and difficulty swallowing and tasting food,” says Hinrichs. “This clinical trial is a first step toward investigating whether T-cell therapy alone, without prior treatments, can eliminate the cancer with fewer long-term side effects.”
Hinrichs anticipates that he and Strauss will be collaborating on future research endeavors. “With the new vaccine trial about to start, our research program is becoming increasingly comprehensive,” he adds. “Now we’ll be better positioned to offer patients different treatment options that should result in even better outcomes.”
Clinicaltrials.gov identifier: NCI-20-C-0104
NCI Protocol ID: NCT04432597
Official Title: HPV Vaccine PRGN-2009 Alone or in Combination with Anti-PDL1/TGF-Beta Trap (M7824) in Subjects with HPV Associated Cancers
The Center for Cancer Research is NCI’s internal cancer center, a publicly funded organization working to improve the lives of cancer patients by solving important, challenging and neglected problems in cancer research and patient care. Highly trained physician-scientists develop and carry out clinical trials to create the medicines of tomorrow treating patients at the world’s largest dedicated research hospital on the campus of the National Institutes of Health in Bethesda, Maryland.
For more information on CCR clinical trials click here, and subscribe to have the latest CCR clinical trials sent directly to your inbox.