As a member of the Translational Immunology Research Program, Staff Scientist Dr. Masashi Watanabe investigates approaches to tailor immunotherapies to treat glioblastomas.
By Raleigh McElvery, Scientific Communications Editor
October 24, 2022
Although the brain and immune system are both crucial for survival, for many years researchers assumed they operated independently. After all, the brain and spine have specialized blood vessels and other cells that form the blood-brain barrier (BBB), which impedes immune cells from easily entering or leaving the central nervous system. This reduces the immune system’s ability to respond to infections or tumors situated in the brain and spine in its usual way.
However, recent studies have revealed that—despite the BBB—an active “dialogue” does persist between the brain and the body’s primary defense network, known as the peripheral immune system. Today, cancer researchers are working to parse these interactions and devise treatments that harness the power of the peripheral immune system to eliminate brain and spine tumors.
Masashi Watanabe, Ph.D., joined the NCI Center for Cancer Research’s Neuro-Oncology Branch (NOB) as a staff scientist in April 2022, hoping to use his expertise in immunology to treat a fast-growing brain tumor called glioblastoma (GBM). It is the most common brain tumor in adults and is known for its ability to resist treatment. As a member of the NOB’s Translational Immunology Research Program led by NOB Chief Mark Gilbert, M.D., Dr. Watanabe investigates how molecules shed from the brain tumor bypass the BBB to activate the peripheral immune system—and how anti-cancer drugs can help mobilize immune cells in the periphery to attack GBM tumors in the brain.
This method of engaging and enhancing a patient’s own immune system to fight cancer is known as immunotherapy. It has gained traction as an alternative to treatments such as chemotherapy, which often destroy healthy cells in addition to cancerous ones. However, to date immunotherapy has been less effective against brain tumors compared to other cancers. By preforming bench-side research in pre-clinical models and aiding in clinical trial development, Dr. Watanabe hopes to design immunotherapies that can easily traverse the BBB to treat brain tumors.
“The exact details of how the brain, brain tumor, and peripheral immune system interact still remain unclear,” he says. “But our research is revealing more and more about this relationship, which will help us transfer new treatments from the bench to the bedside.”
Harnessing T Cells to Tune the Immune Response
As an immunologist, Dr. Watanabe has a long-standing interest in T cells: immune cells that can attack foreign invaders, such as pathogens or tumors. When the peripheral immune system detects a foreign entity, T cells are switched on and molecules called co-stimulatory molecules accelerate their attacking capabilities. When it is time to tamp down an immune response, a similar set of molecules known as co-inhibitory molecules help to turn off the T cells. As a Ph.D. student at the Tokyo University of Science, Dr. Watanabe studied both co-stimulatory and co-inhibitory molecules, which he refers to as the immune system’s “gas pedal and brake.”
After joining the NCI Center for Cancer Research’s Experimental Immunology Branch (EIB) as a postdoc in 2009, Dr. Watanabe continued to probe these same molecules. His primary research projects involved modulating co-stimulatory signals to make vaccines more effective and prevent auto-immune diseases such as multiple sclerosis (when the immune system attacks the brain). At the same time, he also explored how a tumor suppressor gene called p53 affects T cell activation.
In total, Dr. Watanabe spent over a decade at the EIB, and in that time advanced from postdoc to research fellow to staff scientist. In September 2021, he began working part-time at the NOB, and transitioned to a full-time staff scientist seven months later.
“The EIB provided excellent training in basic immunology, but I was anxious to apply my expertise to a clinical setting,” he says. “The NOB is full of researchers with diverse scientific backgrounds—from molecular biology and metabolism to patient outcomes and everything in between—which makes it a very exciting environment to work.”
Although his prior research focused on tamping down the immune response to prevent auto-immune diseases, at the NOB Dr. Watanabe was charged with the opposite task: rallying T cells in the periphery to attack brain tumors. Drugs called immune checkpoint inhibitors (ICIs) do just that by blocking co-inhibitory molecules, known as checkpoint proteins, from switching off T cells. This allows T cells to recognize and kill tumors more efficiently. However, ICIs don’t work very well against brain tumors such as GBM, and Dr. Watanabe aims to change that.
Formulating More Effective Immune Checkpoint Inhibitors
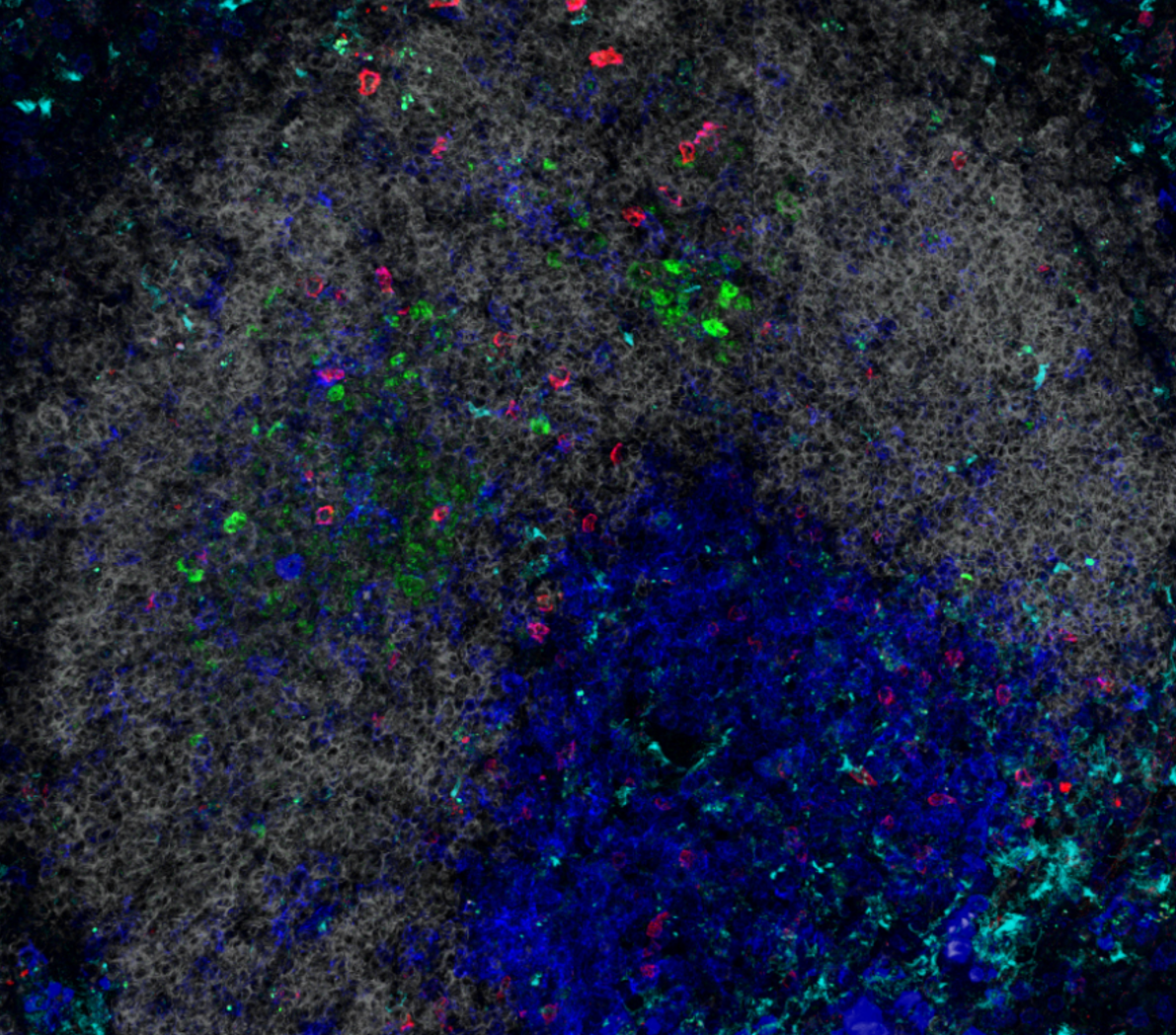
The first step to improving ICIs is to determine why only a small fraction of brain tumor patients respond to this treatment. To answer this question, Dr. Watanabe is using mouse models of GBM to understand how ICIs mobilize T cells in the periphery to breach the BBB—and why some tumors are susceptible to these tactics while others are not.
He is also developing tests that gauge the levels of key molecules in a patient’s blood to pinpoint who is most likely to respond to ICIs. These tests are being evaluated during an ongoing clinical trial at the NOB (NIH Protocol Number 21C0015) that will help doctors determine which patients are likely to respond to immunotherapy and avoid treating those who are less likely to respond. Eventually, this knowledge will also help researchers like Dr. Watanabe design ICIs that work for a broader population of brain tumor patients.
“Most people assume immunotherapy is not an option for these patients,” Dr. Watanabe says. “But we have hope that our work will allow more individuals to benefit. Each new clue brings us closer to understanding how the brain and immune system cooperate—and how to utilize this relationship to fight brain cancer."