Jay A. Berzofsky, M.D., Ph.D.
- Center for Cancer Research
- National Cancer Institute
- Building 41, Room D702D
- Bethesda, MD 20892-5062
- 240-760-6148
- 301-675-0537
- 240-541-4452
- berzofsj@mail.nih.gov
RESEARCH SUMMARY
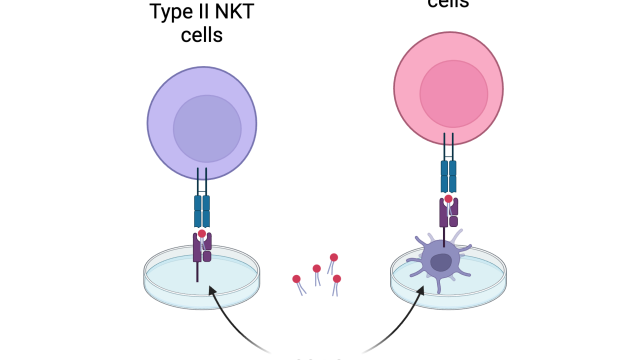
Dr. Berzofsky pioneered characterization of B- and T-cell epitopes and their modification to make epitope-enhanced vaccines and neoepitope vaccines, discovered the importance of T cell avidity in viral/tumor clearance, pioneered use of defined molecular adjuvants to alter quality of immune responses, advanced mucosal HIV and COVID-19 vaccines, discovered NKT cell regulation of tumor immunity, and blocked negative regulation by TGF-beta, IL-13, and regulatory cells to enhance tumor immunity and vaccine efficacy. He translated these strategies to clinical trials in prostate cancer, melanoma, and HER2-positive cancers. As a contractor, he will continue to mentor postdocs and finish publications.
Areas of Expertise
Research
T Lymphocyte Recognition of Antigens and Applications to Vaccines for AIDS, COVID-19 and Cancer
Dr. Berzofsky's lab has focused on elucidating new fundamental principles governing T cell activation, regulation, and effector function, and employing these to develop more effective vaccine and immunotherapy strategies for HIV, cancer, and viruses causing cancer.
Berzofsky pioneered cancer vaccines and immunotherapy, first discovering algorithms to predict T-lymphocyte epitopes, and improve immunogenicity, target neoantigens from mutations and translocations, importance of T cell avidity, use of cytokines to improve immune quality, and a new immunoregulatory NKT-cell pathway controlling tumor immunity, and translating these to the clinic. He pioneered mucosal vaccine strategies for HIV and for SARS-CoV-2 (COVID-19) and tested these in a range of animal models.
Publications
- Bibliography Link
- View Dr. Berzofsky's PubMed Summary.
Mucosal vaccine efficacy against intrarectal SHIV is independent of anti-Env antibody response
Influence of gut microbiome on mucosal immune activation and SHIV viral transmission in naive macaques
Cancer vaccines: translation from mice to human clinical trials
Protection against SARS-CoV-2 infection by a mucosal vaccine in rhesus macaques.
Biography
Jay A. Berzofsky, M.D., Ph.D.
Dr. Jay A. Berzofsky was appointed Chief, Vaccine Branch, Center for Cancer Research, National Cancer Institute, in 2003, after being Chief, Molecular Immunogenetics and Vaccine Research Section, since 1987. He graduated Summa cum Laude from Harvard (1967), and received a Ph.D.-M.D. from Albert Einstein College of Medicine (AECOM). After interning at Massachusetts General Hospital, he joined NIH in 1974. Dr. Berzofsky's research has focused on antigen processing/presentation, epitope structure, cytokine and regulatory cell control of T cell function and avidity, NKT cells, and translation to the design and clinical trials of vaccines for AIDS, cancer, and viruses causing cancer. He has 559 scientific publications. He was elected President of the American Society for Clinical Investigation (1993-94), a member of the Association of American Physicians, a Fellow of the American Association for the Advancement of Science (AAAS), and Distinguished Alumnus of the Year for 2007 by AECOM. He was elected Chair of the Medical Sciences Section of the AAAS for 2007-2008. He received the NIH Director’s Award and the NCI Merit Award in 2008, another NCI Director’s Merit Award in 2011, and a Career Award “for his important contribution to tumor immunotherapy” from the European Academy of Tumor Immunology in 2018.
Dr. Berzofsky retired as Chief of the Vaccine Branch in December 2024.