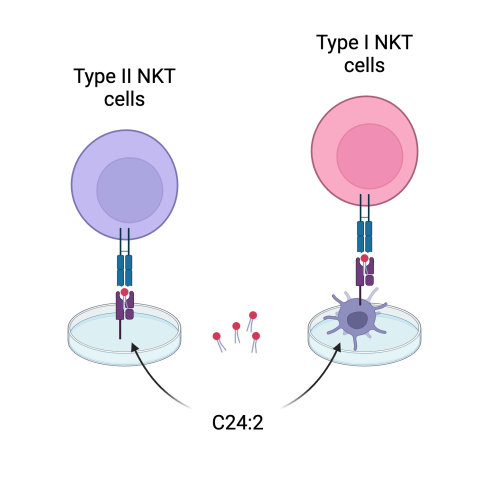
In studying cancer immunotherapies, it is vital to understand how components of the immune system can help or hinder certain immune responses. In lab dish experiments, CCR researchers observed that a lipid molecule called C24:2 (small red dots) activated immunosuppressive type II NKT cells (left, purple) when presented by the CD1d monomers coated on the plastic plate. However, when dendritic cells were added to the dish, these cells took up the C24:2, processed the molecules and displayed them on their own CD1d on their cell surface with a slightly different structure, and activated type I NKT cells, which have an immune-stimulating effect (right, pink). This finding could help researchers design immunotherapies that stimulate the latter type of immune cells for cancer treatment.
Molecules that activate immunity-suppressing cells in a lab dish can become promoters of anticancer immunity when antigen-presenting immune cells alter their structure, CCR scientists have discovered. In mouse experiments, antigen-presenting cells carried out this conversion in the body, creating an immune-activating molecule that protected mice against tumor development.
Jay A. Berzofsky, M.D., Ph.D., Chief of the Vaccine Branch, led the study, which was reported December 21, 2023, in the Journal of Clinical Investigation. The findings could inform the development of new kinds of cancer immunotherapies.
Berzofsky and his team are focused on a component of the immune system called natural killer T (NKT) cells, which recognize and respond to certain lipid molecules. The cells are of interest to cancer researchers because some NKT cells — those considered type I — can trigger an anticancer immune response when they are activated by a certain lipid, known as an antigen. Some lipid antigens, however, activate type II NKT cells, which have an opposite effect: they inhibit anticancer immunity.
To investigate what kinds of molecules are able to activate each type of NKT cell, Kumiko Nishio, M.D., Ph.D., a postdoctoral fellow in Berzofsky’s lab, tested the cells’ response to different lipids in culture dishes. First, Nishio exposed the NKT cells to the lipids by coating the surface of the dish with the molecules. In another experiment, the NKT cells encountered the lipids in a way that more closely resembled what happens in the body: via antigen-presenting cells called dendritic cells. Surprisingly, the same lipid elicited very different NKT cell responses in the two scenarios.
The molecule of interest was a lipid called C24:2, synthesized by Berzofsky’s collaborator Amy Howell, Ph.D., Professor at the University of Connecticut. When coated onto a culture dish, C24:2 activated the immunosuppressive type II NKT cells. When dendritic cells were in the mix, however, they took up the C24:2, processed it into a molecule with a slightly different structure, and then displayed it on their surface, where it activated immune-stimulating type I NKT cells.
“The processing changed them so that they stimulated a completely different T cell and had the opposite effect on tumor growth,” Berzofsky says. “Basically, we were converting a suppressive molecule into a protective molecule.”
Indeed, the team demonstrated that when they injected cancer cells into mice along with C24:2, tumor growth was restricted. The animals’ antigen-processing dendritic cells were essential for this outcome. Understanding and anticipating this processing could help researchers design immunotherapies that stimulate type I NKT cells for cancer treatment.