Terri S. Armstrong, Ph.D., ANP-BC, FAAN, FAANP
- Center for Cancer Research
- National Cancer Institute
RESEARCH SUMMARY
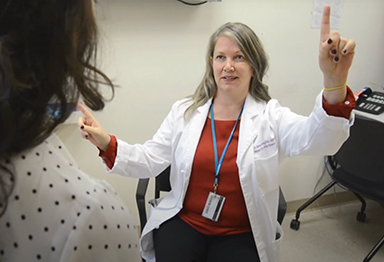
Dr. Armstrong is a trained clinician and scientist, who led the Patient Outcomes Research Program at the Neuro-Oncology Branch (NOB). She strived to understand the impact of both disease and treatment on how a person with a central nervous system (CNS) tumor feels and functions. Driven by her 30 years of experience as a care provider for patients with CNS tumors, she oversaw a research program that primarily investigated this impact through natural history studies, use of patient reported outcomes, and evaluation of interventions that reduced symptom burden. Her research program also included developing preclinical models specifically focused on the effect of circadian dysregulation and sleep alterations on symptomatic toxicities. Additionally, Dr. Armstrong co-led the Cancer Moonshot-funded NCI-CONNECT (Comprehensive Oncology Network Evaluating Rare CNS Tumors) program, which sought to study rare CNS tumors.
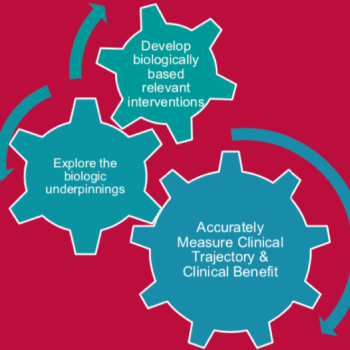
The goal of the Patient Outcomes Research Program is to better understand not only which therapeutic interventions designed at the NOB are beneficial to patient outcomes, but also how these therapies affect the patient themselves. There are several components within Dr. Armstrong’s research that delve deeper into the underlying biology, used technologies and methods that enhance patients’ lives while undergoing treatment, and collected data to gain a better understanding of CNS tumors and their development.
Explore the NOB's Research Programs >
Areas of Expertise
Research
Dr. Armstrong’s Patient Outcomes Research Program is comprised of transdisciplinary research staff and trainees, including research fellows, postdoctoral fellows, pos-baccalaureate fellows, and research associates. Her team brings a translational research approach representing various aspects of patient outcomes research to the Neuro-Oncology Branch (NOB) through preclinical, observational, and interventional studies. Previous studies have shed light on the heavy symptom burden experienced by patients with central nervous system (CNS) tumors, which can lead to functional limitations with significant societal, social, emotional, and financial impacts on their lives.
The first set of studies within Dr. Armstrong’s research program focuses on improving understanding of natural history and outcomes by enrolling every patient that consults with the Branch into the NOB's Natural History Study. Results from this study allow the tracking of each patient’s disease trajectory, and record longitudinal clinician-assessed and self-reported data on symptoms and functions. A standardized collection of patient-reported outcomes is also included in every clinical trial within the NOB, ensuring that the patient-perceived clinical benefit of all therapeutic trials can be measured. Finally, this project also includes the integration of strategic interventions in the form of wearable technologies, mobile application development, and the use of technology to deliver interventions to combat issues—such as scan anxiety or sleep distress—and aid self-management of symptoms.
The second broad project within Dr. Armstrong’s research program explores the identification of clinical and genomic predictors of toxicity. Her previous studies have shown that single-nucleotide polymorphisms can be associated with risk of certain therapeutic-related toxicities occurring with temozolomide use or hypersomnia caused by radiation therapy. Development of mouse models to recapitulate radiation-induced hypersomnia to elucidate their biologic correlates and study circadian rhythms is an additional aim of this work that may eventually improve outcomes in patients. To further this second project, Dr. Armstrong co-leads the NCI-CONNECT (Comprehensive Oncology Network Evaluating Rare CNS Tumors) program with Dr. Mark Gilbert, which aims to advance the understanding of 12 rare adult CNS cancers by establishing and fostering patient-advocacy-provider partnerships and networks to improve approaches to care and treatment. A goal of NCI-CONNECT is to identify clinical and genomic factors associated with the risk of developing toxicities in patients.
Dr. Armstrong’s research program seeks to gain a better understanding of how a patient feels and functions through their disease trajectory. This work can have a significant impact on patients with CNS tumors and their caregivers, affects how a clinician times therapeutic intervention for maximal benefit, and has the potential to improve long-term care for this subset of patients.
Publications
- Bibliography Link
- View Dr. Armstrong's PubMed Summary.
Neurocognitive, symptom, and health-related quality of life outcomes of a randomized trial of bevacizumab for newly diagnosed glioblastoma (NRG/RTOG 0825).
A phase II study of dose-dense temozolomide and lapatinib for recurrent low-grade and anaplastic supratentorial, infratentorial, and spinal cord ependymoma.
Association of circadian clock gene expression with glioma tumor microenvironment and patient survival.
Glioma patient reported outcome assessment in clinical care and research: a RANO collaborative report.
See brain cancer as more than just the sum of biology.
Biography
Terri S. Armstrong, Ph.D., ANP-BC, FAAN, FAANP
Dr. Armstrong obtained a Bachelor of Science in nursing from the University of Akron in Ohio, a Master of Science in oncology from Ohio State University, a Postmaster’s Nurse Practitioner Certificate, and was soon after introduced to the field of neuro-oncology. Realizing that her passion lay in understanding disease burden for patients and their caregivers, she became an instructor and adjunct faculty member at Emory University, where her experience drove her to later pursue a Ph.D. and eventually lead an independent research program. Dr. Armstrong remained an advanced practice nurse and adjunct faculty member at The University of Texas MD Anderson Cancer Center (MDACC) while working on her advanced degree. Upon completion, she joined the faculty at The University of Texas Health Science Center while maintaining an adjunct position at MDACC as an associate professor. She was awarded the John S. Dunn Distinguished Professorship in Oncology Nursing in 2012, followed by tenure. In 2016, she joined the Neuro-Oncology Branch (NOB) as a tenured senior investigator and head of the Patient Outcomes Program. She also served as the NOB’s deputy chief from 2018 to 2024 and is licensed to practice as a clinician in Maryland.
In addition, Dr. Armstrong has served on several NIH and professional committees, including the past vice president of the Society for Neuro-Oncology (SNO). She has also held multiple positions on SNO’s board of directors, in addition to being an elected member and chair of the NCI’s Center for Cancer Research Women Scientist Advisors. She was the executive editor for Neuro-Oncology Practice and former associate editor for several other journals, such as Neuro-Oncology. Her work is highlighted by an impressive track record of awarded grants—including grants from the CERN (Collaborative Ependymoma Research Network) Foundation, the National Institute of Nursing Research R01-funded grant, and a Beau Biden Cancer Moonshot grant received in 2017 that provided the funding for the NCI-CONNECT (Comprehensive Oncology Networks Evaluation Rare CNS Tumors) program.
Dr. Armstrong retired in September 2024 and is now an NIH Scientist Emeritus.
Honors, Awards and Leadership
- NCI Director’s Champion Award - 2022
- NCI Director’s Award - 2020, 2021
- NCI Director’s Emerging Leader Award - 2020
- Distinguished Alumni, University of Texas Health Science Center - 2018
- Dean’s Mentoring Award, University of Texas Health School of Nursing - 2015
- Inducted Fellow, American Academy of Nursing - 2013
- John S. Dunn Distinguished Professorship in Oncology Nursing, University of Texas Health School of Nursing - 2012
- Inducted Fellow, American Academy of Nurse Practitioners - 2009
- Outstanding Researcher of the Year, Sigma Theta Tau - 2008
- Doctoral Student Writing Award, University of Texas Health School of Nursing - 2006
- Patient Educator of the Year, MD Anderson Cancer Center - 2005
- Educator of the Month, MD Anderson Cancer Center - 2005
- Leadership Award in Education, MD Anderson Cancer Center - 2001
- Quality of Life Lectureship, Oncology Nursing Society - 1998
- Phi Kappa Phi Scholastic Honor, Ohio State University - 1991
Select Societies and Initiatives
- Chair, NCI Center for Cancer Research (CCR) Clinical Trial Diversity Committee - 2021-present
- NCI Center for Cancer Research (CCR) Women Scientist Advisory Committee - 2018-present
- Collaborative Ependymoma Research (CERN) Foundation Board Member - 2015-present
- NCI Equity and Inclusion Committee - 2021-2023
- NCI Center for Cancer Research (CCR) Scientific Advisory Board - 2021-2023
- Society for Neuro-Oncology: Annual Awards Committee (2007-2015), Board of Directors (2008-2011), Vice President (2015-2017), Health Policy Committee Chair (2015-2018), Guidelines Committee (2016-present), Wellness Committee Co-Chair (2018-2020)
- Patient Reported Outcomes Committee, NRG, NCI - 2014-2019
- Head for the Cure Board of Directors - 2012-2016
- American Society of Clinical Oncology (ASCO), PLWC Advisory Panel - 2006-2017
- Alliance Oncology Research Group: Health Disparities (2013-present), Neuro-Oncology Working Group (2013-present), CCDR Representative for Neuro-Oncology (2013-present)
News
Celebrating CCR Careers: Terri Armstrong, Ph.D.
Dr. Terri Armstrong will be retiring after eight years at the Neuro-Oncology Branch, leaving behind a legacy of insightful patient outcomes research and exceptional patient care. Read more >
Smart Wearables Show Promise for Tracking Sleep Patterns in Brain Tumor Patients
An interim study analysis demonstrates that combining Fitbit data with self-assessments is a reliable method for understanding sleep changes in patients. Read more >
Examining Social Determinants of Health to Improve Brain Tumor Patient Quality of Life
June 24, 2024
A new study explores how non-medical factors influence the neurocognitive and mood-related symptoms that people with brain tumors experience. Read More >
Forming Connections to Address Rare Brain Tumor Treatment and Care
May 21, 2024
Scientists and neuro-oncology providers are taking a comprehensive approach to improve care and treatment—performing laboratory research, conducting clinical trials, and fostering a sense of community. Watch Now >
Study Finds Genetic Mutation Combats Daytime Sleepiness Caused by Brain Cancer Treatment
November 8, 2023
Preclinical experiments reveal that an alteration in the circadian PER2 gene may help prevent some of the negative side effects that brain tumor patients experience from radiation therapy. Read more >
Center for Cancer Research Hosts Communications Course for Healthcare Providers in Oncology
August 9, 2023
Over 20 people from various oncology disciplines gathered to learn how to better communicate with patients and families about critical aspects of care. Read more >
Advancing the Science of Survivorship in Neuro-Oncology
May 12, 2023
Dr. Terri Armstrong joined fellow leaders in the field of cancer survivorship to discuss the needs of those living with brain and spine tumors, as well as goals for the future and research funding opportunities. Read more >
Neuro-Oncology Branch Members Earn NCI Director’s Awards for Improving Patient Care and Outcomes
April 5, 2023
Dr. Terri Armstrong, Alvina Acquaye-Mallory, and Tracy Ani were recognized for their efforts to make clinical trials more inclusive, while Dr. Jing Wu was recognized for her research on the anticancer drug zotiraciclib. Read more >
Natural History Study for Rare Brain and Spine Tumors Enrolls One Thousand Participants
November 17, 2022
In the six years since it began, the Natural History Study has amassed an enormous database of information that is helping to improve treatment and quality of life for patients with rare central nervous system cancers. Read more >
August 4, 2022
Summer interns investigated methods to improve immunotherapy, tailor survivorship programs, and target cancer cells using antibiotics. Read more >
Improving Everyday Life for People with Rare Brain and Spine Cancers
Dr. Terri Armstrong shares why she chose to study rare brain and spine tumors and how her research is advancing patient quality of life. Read more >