This will be the first of several articles that describe the types of experiments that laboratory researchers perform and the starting materials that are required.
Not only is a tumor sample important, but it is one of THE MOST IMPORTANT resources that a laboratory researcher can have. Please keep this in mind when reading this article.
If we could grow a tumor in a dish in the laboratory, we could ask questions like, what makes it grow? And even more importantly, what makes it stop growing? But we have not been able to grow tumors in this way from patients with wildtype GIST. Part of this is because the number of samples is small, due to the rarity of pediatric and wildtype GIST. Another problem may be that they are just difficult to grow.
The process of growing tumors in the laboratory is very similar for all types of tumors. Since we do not have an example of a wildtype GIST tumor, we will explain the process for a bone tumor called osteosarcoma.
When a surgeon takes out your tumor, it goes to doctors in the pathology department. Pathologists look at the tumor under a microscope to identify what type of tumor it is. After they are certain that they do not need any more of the sample to make decisions about your care, they may store it, and they may also give some of the sample to laboratory researchers, if requested.
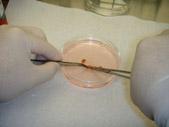
When researchers (will henceforth be referred to as, we) obtain a piece of the tumor we prepare it to be able to grow in a dish. Shown on the right is a photograph of a portion of the lung (red) contained in a transparent circular container (Picture 1). The pen is there to provide a sense of the actual size. If you look closely, there are several white dots on the lung surface, three of which are larger than the others. You can move the cursor over the picture to see a magnified view. These spots are all part of a bone tumor that has spread to the lung. We then process this specimen to allow the tumor to grow in a dish.
We use surgical scissors (Picture 2) and then a sharp scalpel to mince the tumor into very small fragments (Picture 3). We then add it to a container, known as a tissue culture flask (Picture 4). This flask is coated with a material that helps cells stick to the inner surface, providing them a better surface to grow on. We then add a pink liquid that is called tissue culture media. This contains all of the nutrients that are present in a healthy diet that will allow the tumor to grow.
We then place the flask into a tissue culture incubator (Picture 5 and Picture 6). The incubator is calibrated with gases and heat to mimic the conditions in the human body as closely as possible. The temperature is 98.6 degrees Fahrenheit (the same temperature as the inside of our bodies). The oxygen level is 21% (the amount in the air that we breathe in). The carbon dioxide level is 5% (the same as the amount that we exhale). All of these steps are performed in a surgically sterile environment that prevents bacteria, fungus and anything else that may contaminate and destroy the sample.
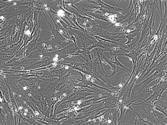
The small chunks of tumor that we cut up earlier settle on the bottom of the tissue culture flask. Then, they start to shed cells that attach to the flask. The photograph below was taken using a microscope and shows a small tumor chunk (brown ball) that has shed some cells that are now growing on the inside surface of the tissue culture flask (Picture 7). These cells can be tumor cells. But many times they are long thin cells called fibroblasts, which are normal cells in the body, in this case the lung (Picture 8).
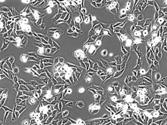
In most cases, the only cells that grow are the normal fibroblasts. Rarely, tumor cells will also grow (Picture 9). Sometimes, it may take up to one year for the tumor cells to start growing. When they do, we call it a tumor cell line. At this point, we can keep growing these cells indefinitely. Tumor cell lines provide one of the most important resources that researchers have, in their efforts to study why tumors form, and how to prevent their growth (Experiments That We Can Perform Using Tumor Cell Lines). At the NIH, and at all CPGR institutions, we attempt to establish a cell line from all samples that have been surgically removed for all patients with pediatric tumors.
What Can I Do to Help?
If you are about to undergo removal of a tumor, please inform your doctor that you would like any tumor sample that is left over to be used for research. Let them know specifically that you would like the tumor to be made into a cell line, to be implanted into a mouse (Article 3), to be frozen (Article 4) and to be stored for other studies. The NIH can provide any instructions if needed.
As you read other installments of these research articles, you will see that there are many things that you can do to help laboratory scientists.
Frequently Asked Questions About This Article
Can I send my tumor sample to the NIH to have a cell line generated?
Unfortunately, no. Dr. Lee Helman studied the possibility of attempting to develop cell lines from tumor samples that were sent from around the nation for a bone tumor called Ewing’s sarcoma. Patients who had surgery, had a portion of their tumor placed into a tube containing tissue culture media, which was then shipped by priority overnight delivery to his laboratory at the NIH. A laboratory technician then performed the steps described above. Of 52 samples that were sent, no cell lines were established. Over that same time period, 14 patients underwent surgery at the NIH. Of these 14 samples, 4 were successfully made into cell lines. Compared to a 0% success rate for samples shipped overnight, there was a 28% success rate if the process was started immediately. This study demonstrated the importance of initiating the process as quickly as possible, from the time of surgical removal, to the time that the tumor fragments are placed in the incubator. Therefore, this procedure can only be performed at the hospital in which the surgery takes place.
Can someone at my hospital generate a cell line from my tumor?
Yes. Almost all research hospitals have the capability to perform tissue culture. If your oncologist or surgeon can identify a tissue culture facility and someone who has experience in performing tissue culture, it should be possible. The NIH would be happy to provide any information and advice.
Can you use a cell line from my tumor to make decisions about my treatment?
Definitely not, for many reasons. Practically, no one has been able to establish a cell line from a pediatric or wildtype GIST tumor sample yet. Second, it may take up to one year to establish these cell lines and treatment decisions cannot wait that long. Third, and most importantly, it is unclear if the cell line exactly represents your tumor. It is possible that some other changes occurred to the cells during the long processing time. Tumor cell lines make great laboratory research tools (Experiments That We Can Perform Using Tumor Cell Lines), but they should never be used to make treatment decisions.
Click here if you would like to ask a question about this article.