CCR researchers showed that engineered natural killer cells (yellow) can expand in solid tumors and kill tumor cells (red).
With genetic engineering, stem cells can be directed to generate natural killer cells — a type of immune cell — that can destroy solid tumors, CCR scientists have found. The research, led by Raffit Hassan, M.D., Senior Investigator in the Thoracic and GI Malignancies Branch, and Qun Jiang, Ph.D., a staff scientist in his lab, was reported May 2, 2025, in Science Advances.
As researchers work to develop cellular immunotherapies to treat solid tumors, some are seeking a more streamlined approach than the highly personalized T-cell therapies. Cancer-targeting natural killer cells have emerged as a promising alternative.
T-cell based immunotherapies are created from patients’ own T cells because foreign T cells could attack the body’s own tissues when delivered to a patient, Jiang explains. In contrast, natural killer cells do not. That means natural killer cell–based therapies can be developed in bulk from cells that came from healthy donors and delivered to patients without the risk of graft-versus-host disease. Researchers often call this type of treatment an “off-the-shelf” product, in contrast to highly personalized treatments like chimeric antigen receptor (CAR) T-cell therapies.
Still, equipping natural killer cells with receptors to guide them to their targets, then growing the engineered cells in a lab until they generate sufficient numbers for therapy, is complex and time-consuming. The most efficient method involves genetically programming stem cells to produce the receptor, then directing those stem cells to develop into natural killer cells. Stem cells are also a consistent, homogeneous source of starting material that allows for quality control and large-scale, cost-effective manufacturing.
To accelerate production, Jiang and her colleagues introduced two key features into the stem cells. The first was a CAR that recognizes the protein mesothelin, which is abundant on the surface of many solid tumors. The second was IL-15, which promotes natural killer cells’ development, proliferation and activation. By including the IL15 gene, the team dramatically increased the rate at which the stem cells developed into natural killer cells.
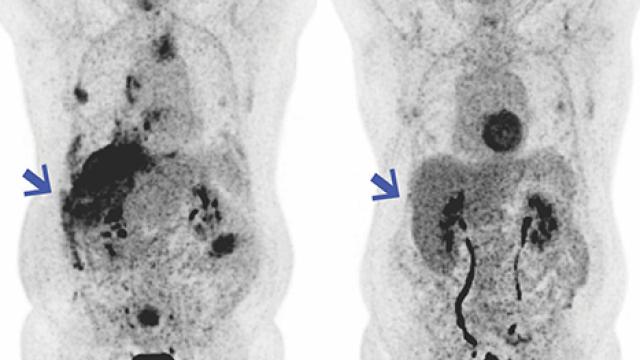
The team tested these natural killer cells against a variety of cancer cells, both in laboratory dishes and animal models. In experiments with pancreatic, gastric and ovarian cancer cells as well as mesothelioma cells, the engineered immune cells efficiently killed their targets. In mice, they effectively infiltrated and shrank tumors.
Hassan says a key to the cells’ ability to home in on their targets efficiently is the particular mesothelin-recognizing antibody that the team incorporated into the cells’ CAR. This antibody was developed by his CCR collaborators in the Laboratory of Molecular Biology: Mitchell Ho, Ph.D., Deputy Chief, and Ira Pastan, M.D., NIH Scientist Emeritus. Another key factor that enhances natural killer cell effectiveness is the expression of IL-15, which supports the cells’ persistence within the tumor environment.
Guided by findings from the new study, Hassan’s team will continue refining natural killer cells to improve their ability to control solid tumors before undertaking clinical testing. A priority, he says, is ensuring that therapeutic cells will persist inside the body long enough to carry out a sustained attack.