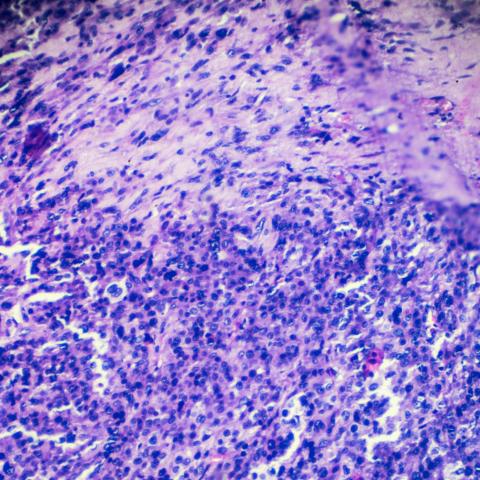
Rhabdomyosarcoma biopsy under microscopy. CREDIT: jxfzsy/iSTOCK
A recent study testing a chimeric antigen receptor (CAR) T-cell therapy for rhabdomyosarcoma in mice shows that the therapy could effectively eliminate the vast majority of tumors in a matter of weeks. The results, published in Cell Reports Medicine on September 21, 2023, pave the way for the therapy to be tested in humans in a phase I clinical trial.
Rhabdomyosarcoma is the most common soft tissue sarcoma affecting children. Up to 20 percent of patients with low-risk disease and more than 70% with high-risk disease do not respond to standard treatment and may die from the disease, despite a combination of surgery, radiation and aggressive chemotherapy.
Javed Khan, M.D., Senior Investigator in the Genetics Branch, postdoctoral researcher Meijie Tian, Ph.D., their team and collaborators have been exploring the possibility of using CAR T-cell therapy to treat rhabdomyosarcoma. CAR T-cell therapy is a type of immunotherapy that involves taking cancer-fighting immune cells, called T cells, from a patient and genetically engineering them to target a specific protein found on the surface of cancer cells. The modified T cells are then injected back into the patient, with a boosted ability to fight cancer.
Khan’s team previously identified a protein, FGFR4, that is highly expressed on the surface of rhabdomyosarcomas. Subsequently, they developed a CAR T-cell therapy capable of targeting the protein, called 3A11 CAR T cells.
In the study, the researchers first conducted experiments in petri dishes showing that the engineered 3A11 CAR T cells targeted and killed human cancer cells, but did not react against healthy cells, suggesting it could be a safe therapy for further testing.
Next, they injected the CAR T cells into mice with two different subtypes of rhabdomyosarcoma. The results showed that mice treated with the CAR T cells had a significantly lower tumor burden compared to untreated mice and mice that were treated with unaltered T cells. After 42 days, almost all mice treated with the new CAR T cells survived and were tumor-free, whereas the untreated mice did not survive.
“It was really exciting to see these results,” says Khan. “Previously, clinical trials in humans and mice with widespread rhabdomyosarcoma have been ineffective, but the CAR T-cell therapy produced a dramatic response I have never seen before.”
Khan is currently working with the U.S. Food and Drug Administration and the Pediatric Oncology Branch to launch a phase I clinical trial to test this novel therapy in patients between the ages of 3 and 30 with aggressive rhabdomyosarcoma that has not responded to conventional therapies.
“We have a great deal of work ahead, but the hope is that this therapy is going to work for people with this type of cancer that has been unresponsive to other treatments,” says Khan.