Dr. Vivian De Alvarenga Guedes is studying the molecular events underlying brain tumor symptoms—and how biological age affects these symptoms—to discover new ways to improve them.
By Kendall Morgan, Neuro-Oncology Branch Contributor
June 28, 2023
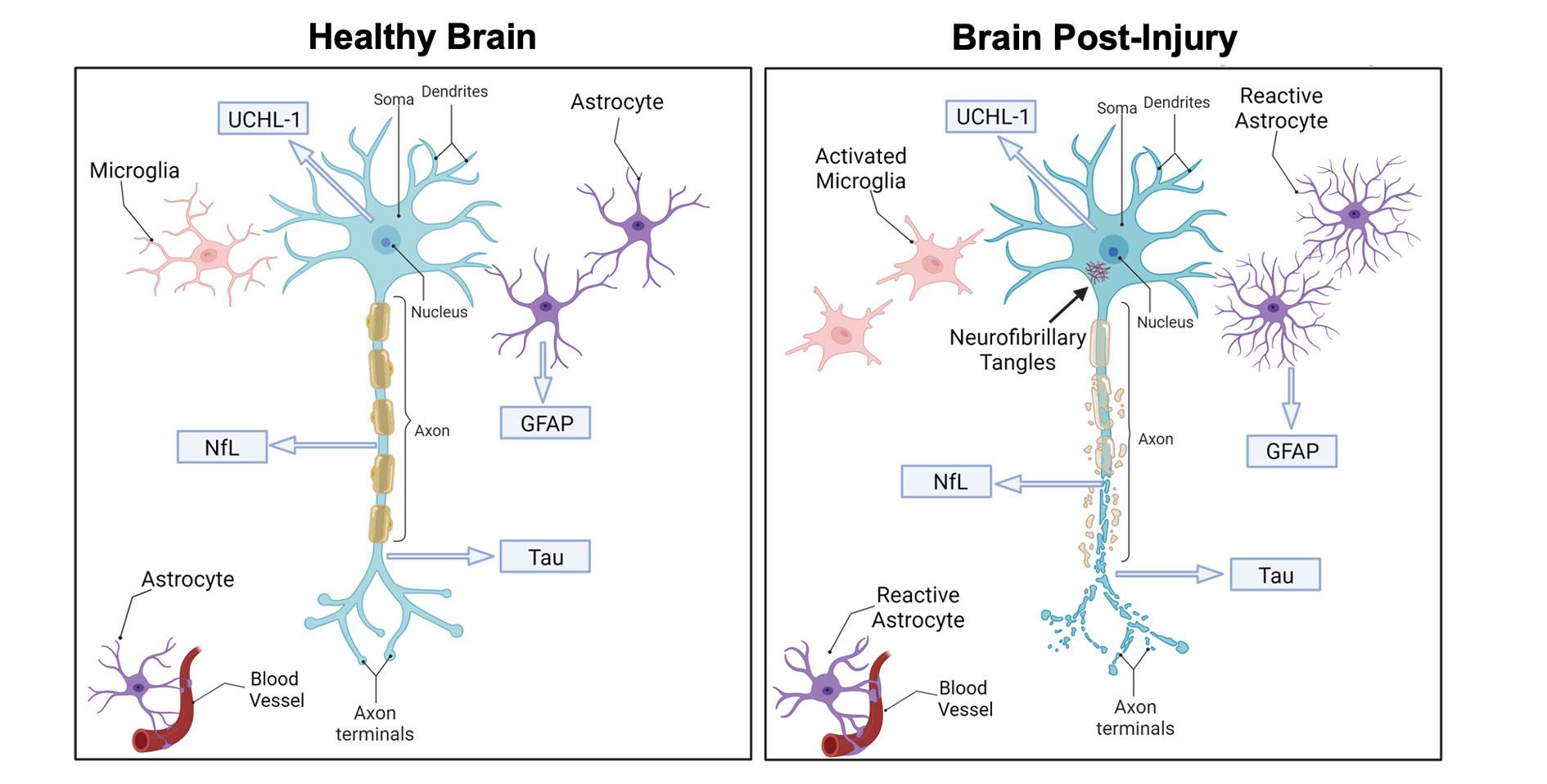
Before joining the NCI Center for Cancer Research’s Neuro-Oncology Branch (NOB) in July 2022 as a staff scientist, Vivian De Alvarenga Guedes, Ph.D., didn’t study cancer. Instead, she focused on traumatic brain injuries—a different sort of brain ailment that taught her how to understand patients’ lived experiences and relate them to measurable molecular “signatures.” These signatures, also called biomarkers, are invisible to the naked eye but can be captured in blood tests.
In her new role at the NOB, Dr. Guedes is applying her unique expertise to dig deeper into the symptoms that people with brain tumors experience. She’s in search of sophisticated new ways to monitor patients and improve care.
“If we can associate these molecular signatures with the symptoms a person reports—whether these symptoms are due to traumatic brain injury or a brain tumor—the hope is that we can better understand what mechanisms underlie the symptoms and potentially find ways to intervene,” Dr. Guedes says.
Finding Signatures of Brain-Related Symptoms
Dr. Guedes’s previous work as a research fellow at the NIH’s National Institute of Nursing Research (NINR) focused on the long-term outcomes associated with traumatic brain injuries. She analyzed vast quantities of clinical data describing the symptoms experienced by military service members, veterans, college athletes, and other brain trauma patients. The goal was to integrate all that clinical data and relate it in meaningful ways to the molecules she could measure in those individuals’ blood samples. Dr. Guedes says that her time at NINR helped expand her earlier background in basic neuroscience and preclinical studies to embrace a more patient-focused perspective.
She found, for instance, that those with a history of repeated mild brain injuries still have unique molecular signatures in their bloodstream even years later. What’s more, those with significant molecular evidence of neuronal injury and inflammation also had the most severe symptoms. These may include problems with concentration or memory, as well as depression.
Now, as a member of the NOB’s Patient Outcomes Research Program led by NOB Deputy Chief Terri Armstrong, Ph.D., Dr. Guedes thinks pinpointing biomarkers of brain cancer could unlock important clues for understanding brain tumor symptoms.
Studying Brain Tumors and Aging
Dr. Armstrong’s Patient Outcomes Research Program strives to understand the impact of both cancer and its treatment on how a person with a central nervous system (CNS) tumor feels and functions. The lab examines not only which therapeutic interventions designed in other parts of the NOB are beneficial to patient outcomes, but also how they affect patients in a more holistic way. To move those ongoing efforts forward, Dr. Guedes says she is developing a “new area of research” in the lab—unpacking a person’s complex, underlying molecular layers to understand how they’re associated with changes in cognition and other symptoms.
In one of her first projects at the NOB, Dr. Guedes is exploring the links between brain tumor symptoms and aging in data and samples collected in the Natural History Study—a large and long-running observational study that follows patients to understand what life is like across their entire cancer trajectory.
When Dr. Guedes says she studies aging, she doesn’t just mean a person’s chronological age measured in years. She studies biological age—chemical changes to DNA that may happen at different rates depending on life experiences, including cancer. Biological age can affect how a person feels and functions regardless of how old their driver’s license says they are. She suspects that CNS cancers and their treatment may effectively make a person biologically “older” than they otherwise would be.
A person’s chronological age affects symptoms and response to treatment, Dr. Guedes says. “At the same time, we also believe that a brain tumor and its treatment might cause biological aging of the person. Your chronological age and biological age are not necessarily the same.”
The question Dr. Guedes wants to answer is whether patient-reported symptoms and outcomes are influenced by both chronological age and biological age. In particular, she wants to determine if brain tumors accelerate the aging process in ways she can measure. It’s an especially important issue, she notes, because biological aging may change patient outcomes and the way a person responds to and recovers after cancer treatment.
Bringing It All Together
In future work, Dr. Guedes will also apply cutting edge approaches to measure molecules in the bloodstream, including those contained inside miniature sacs that can cross out of the brain and into the bloodstream. Known as extracellular vesicles (EVs), these tiny sacs are especially useful for the study of brain injury and brain diseases such as cancer. That’s, in part, because the membranes that surround them protect their contents from being broken down by enzymes. It’s also possible to trace EVs back to the specific tissues or organs they originally came from by looking at proteins on their surfaces. All these attributes of EVs make it easier to tell from a blood sample what’s happening in the brain.
“Extracellular vesicles are like little packages,” Dr. Guedes explains. “If you can isolate them in the blood, you can look inside the package to analyze the molecules there. They can give you a more complete story of what is happening inside the body in response to disease.”
Ultimately, Dr. Guedes is applying her expertise in neuroscience, biomarker development, and understanding patient symptoms to support the overarching goal of the NOB’s NCI-CONNECT program, which aims to advance the understanding of rare adult CNS cancers to improve care and treatment.
“The idea is to bring it all together,” she says. “If I can integrate my previous experience with molecular mechanisms and analysis of clinical samples with the patients who are right there in front of us, that’s important and powerful.”