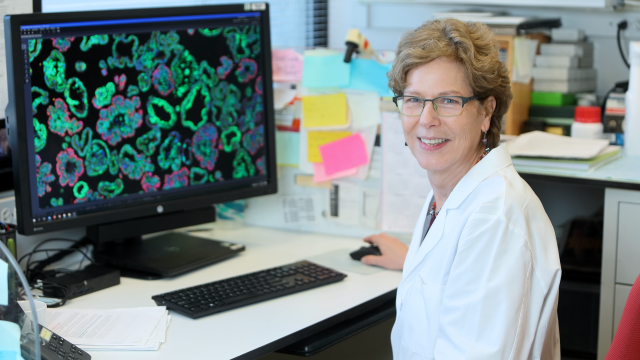
Kathleen Kelly, Ph.D.
- Center for Cancer Research
- National Cancer Institute
RESEARCH SUMMARY
Dr. Kelly’s program investigated mechanisms of prostate cancer tumorigenesis and progression. A major area of focus addressed the roles of oncogenotype, tumor heterogeneity/cancer stem cells, and metabolism in the development of therapeutic responses, especially for castrate-resistant prostate cancer. Additional research investigated signal transduction pathways that influenced prostate cancer bone metastasis. As chief of LGCP, Dr. Kelly advanced integration with the clinical prostate cancer program to carry out mechanism-based translational studies using a variety of pathological, genomic, and patient-derived live culture approaches.
Areas of Expertise
Research
Research Interests
Our laboratory focused on understanding the mechanistic consequences of specific genetic alterations that lead to the development of prostate cancer (PC), especially as related to progression. Prostate cancer (PC) is the most frequently diagnosed non-cutaneous cancer in men, and although organ confined PC is highly treatable with surgery and/or radiation, metastatic disease is incurable and leads to significant morbidity and mortality. Our goal was to improve detection and treatment of prostate cancer through understanding genomic and biochemical mechanisms of disease progression.
We used two complementary approaches, patient-derived xenografts/organoids and genetically engineered mouse models (GEMMs). A strength of our laboratory was our ability to employ a wide variety of in vivo models and imaging modalities. We used the large cohort of LuCaP patient-derived CRPC xenografts established by our collaborators at the University of Washington. The LuCaP cohort represents the genotypic and phenotypic heterogeneity of advanced prostate cancer clinical samples. To facilitate experimental manipulations, including genetic modifications and high throughput screening assays, we optimized organoid methods for establishing and maintaining in vitro cultures of LuCaP xenograft tumor cells. In addition to the LuCaP organoids, we also developed a number of organoid cultures from NIH clinical center CRPC patient biopsy samples. Together these organoid cultures in combination with matching PDX tumors provide an extensive, clinically-relevant experimental platform. One major effort was focused upon high throughput screens to determine therapeutic sensitivity and metabolic characteristics (including imaging tools) as they relate to molecular characteristics. A second effort addressed the genetic and epigenetic mechanisms of CRPC dedifferentiation and neuroendocrine transdifferentiation that occurs in response to androgen deprivation.
GEMMs are particularly useful for the availability of genetically-defined tumor tissue, the ability to longitudinally investigate various stages of prostate cancer progression, and the ease of manipulating the hormone environment. Models of aggressive CRPC in mice have provided insight into poorly differentiated tumors enriched for cancer stem/progenitor cells. Combined PTEN/TP53 mutations occur in ~30% of clinical CRPC. Our characterization of a Pten/Tp53 null prostate cancer GEMM model revealed that the amplification and plasticity of luminal prostate cancer progenitor cells contributes to the aggressive and castration resistant nature of the disease. Other investigations were focused upon the signaling pathways that promoted self-renewing cancer stem cells and their relationship to castration indifference.
Publications
- Bibliography Link
- View Dr. Kelly's PubMed Summary
TMPRSS2-ERG promotes the initiation of prostate cancer by suppressing oncogene-induced senescence
EGR1 regulates angiogenic and osteoclastogenic factors in prostate cancer and promotes metastasis
A PDX/organoid biobank of advanced prostate cancers captures genomic and phenotypic heterogeneity for disease modeling and therapeutic screening
Platelets Promote Metastasis via Binding Tumor CD97 Leading to Bidirectional Signaling that Coordinates Transendothelial Migration
Androgen deprivation leads to increased carbohydrate metabolism and hexokinase 2-mediated survival in Pten/Tp53-deficient prostate cancer
Biography
Kathleen Kelly, Ph.D.
Dr. Kelly received her Ph.D. from the University of California, Irvine. She completed her postdoctoral training in the laboratory of Philip Leder, Harvard Medical School, and she maintained an independent research program at the NCI from 1984 to 2023. Dr. Kelly's interests were focused on the genetic regulation of cell growth, cancer progression and metastasis. She served as branch chief from 1997 to 2023, and a CCR Deputy from 2019-2023. Dr. Kelly retired in December 2023 and is now an NIH Scientist Emeritus.
News
Alumni
Lab Life

Kelly Lab 2022

Holiday Party 2021

Holiday Party 2021
Kelly Lab 2019
Keith's Farewell
Kelly Lab 2017
Franks's Farewell Party
Kelly Lab 2017
John's Farewell 2017
John's Farewell

Yvona's Farewell Party
Yvona's Farewell Party

Yvona's Farewell
Kelly Lab 2016
Lauren's Farewell
Kelly Lab 2015
Caitlyn's Farewell 2015
Amir's Farewell 2014
Kelly Lab 2014

2014 Relay Race
Kelly Lab 2014
Paul's Farewell
Paul's Farewell
Paul's Farewell
Paul's Farewell
Kelly Lab 2013
Orla's Farewell
Orla's Farewell
Orla's Farewell Party
Orla's Farewell Party
Kelly Lab 2012
Jake's Farewell
Wassim's Farewell 2011
Kelly Lab 2011
Wassim's Farewell
Wassim's Farewell

Victoria's Farewell

Victoria's Farewell

Victoria's Farewell

Kelly Lab 2007