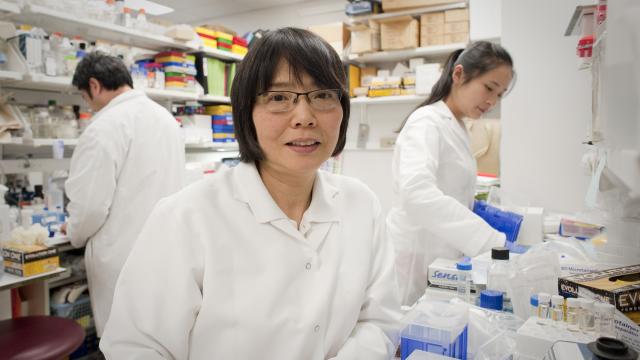
Shioko Kimura, Ph.D.
- Center for Cancer Research
- National Cancer Institute
- Building 37, Room 3112B
- Bethesda, MD 20892
- 240-760-6877
- kimuras@mail.nih.gov
RESEARCH SUMMARY
Dr. Kimura’s research focused on understanding the role of homeodomain transcription factor NKX2-1, a marker for lung adenocarcinoma in humans, and its downstream target, a novel cytokine-like immunomodulatory protein, secretoglobin (SCGB) 3A2, in development, function, homeostasis, and physiology of the thyroid and lung, and pathogenesis of diseases, including cancers of these organs. Dr. Kimura used cell culture and mouse models with various genetically engineered mouse lines to investigate these problems.
Areas of Expertise
Research
Role of NKX2-1 in thyroid regeneration and carcinogenesis
NKX2-1 is a critical transcription factor for the genesis of thyroid, lung, ventral forebrain, and pituitary, and is essential for the maintenance of normal architecture and function of the differentiated thyroid as demonstrated by Nkx2-1-null and Nxk2-1-thyroid specific conditional-null mice, respectively. Our previous research suggested that NKX2-1 may be related to the maintenance and/or activity of thyroid stem/progenitor cells, the disturbance of which leads to thyroid carcinogenesis, and a balance of expression/no-expression of NKX2-1 may be critical if a thyroid differentiates or proceeds to carcinogenesis. It is known that in thyroid cancers, the degree of dedifferentiation generally correlates with the decreased level of NKX2-1 expression.
Our recent research focused on the role of NKX2-1 in thyroid regeneration using partial thyroidectomy mouse model with the hypothesis that the stem/progenitor cells may be activated under partial thyroidectomy. We found that a cluster of thin and elongated shaped NKX2-1-positive cells were found located near the tracheal cartilage and muscle, some of which were connected to a newly formed follicle-like structure with round shaped NKX2-1 positive cells. Experiments were carried out to understand the nature of NKX2-1-positive cluster of cells that appear after partial thyroidectomy.
Role of novel cytokine-like immune modulatory molecule secretoglobin (SCGB) 3A2
SCGB3A2 was initially identified as a downstream target for NKX2-1 in lung by suppressive subtractive hybridization method using Nkx2-1-null vs. wild-type mouse embryo lungs. SCGB3A2 is predominantly expressed in lung, with only very weak expression in the thyroid. We demonstrated multiple SCGB3A2 functions in the lung; 1) Anti-inflammatory activity initially by administration of adenovirus expressing SCGB3A2 to the ovalbumin allergic airway inflammation model mice, later by use of Scgb3a2-null mice. 2) Growth factor activity promoting embryonic lung development and branching morphogenesis using ex vivo embryonic lung organ culture and in vivo administration of recombinant SCGB3A2 to pregnant female mice, 3) Anti-fibrotic activity using bleomycin-induced pulmonary fibrosis model mice with the administration of SCGB3A2 protein, and by use of Scgb3a2-null and Scgb3a2-lung-specific overexpressing transgenic mice, 4) Airway and carcinoma markers, 5) Anti-cancer activity, and recently 6) anti-emphysematous activity. For the anti-cancer activity of SCGB3A2, we identified syndecan-1 (SDC1), a member of the transmembrane heparan sulfate (HS) proteoglycan family, as a SCGB3A2 receptor by use of human protein-protein interaction microarrays. SCGB3A2 is an LPS-binding protein and chaperones LPS to cell cytosol through SCGB3A2-LPS complex binding to SDC1. Internalized LPS is a known activator of the non-canonical inflammasome pathway, that leads to inflammatory cell death, also known as pyroptosis. We discovered that cells expressing SDC1 on their cell surfaces with abundant HS and caspase-4 (CASP4), the critical molecule in the non-canonical inflammasome pathway, regardless of origins of cancers, are susceptible to SCGB3A2-induced growth inhibition in the presence of LPS in vitro and in in vivo xenograft model mice. Our recent research focused on 1) To determine the extent of SCGB3A2/LPS-induced cell growth inhibition using various cancer cell lines derived from many different organs, and 2) To understand the tumor microenvironment affected by SCGB3A2. This project emphasized the translational aspect of research, which leads to development of SCGB3A2 as a therapeutic to treat cancers.
Publications
- Bibliography Link
- View Dr. Kimura's Complete Bibliography at NCBI.
Secretoglobin 3A2 eliminates human cancer cells through pyroptosis
A novel pathway of LPS uptake through syndecan-1 leading to pyroptotic cell death
An in vivo model for thyroid regeneration and folliculogenesis
Preclinical evaluation of human secretoglobin 3A2 in mouse models of lung development and fibrosis
Nkx2-1 represses a latent gastric differentiation program in lung adenocarcinoma
Biography
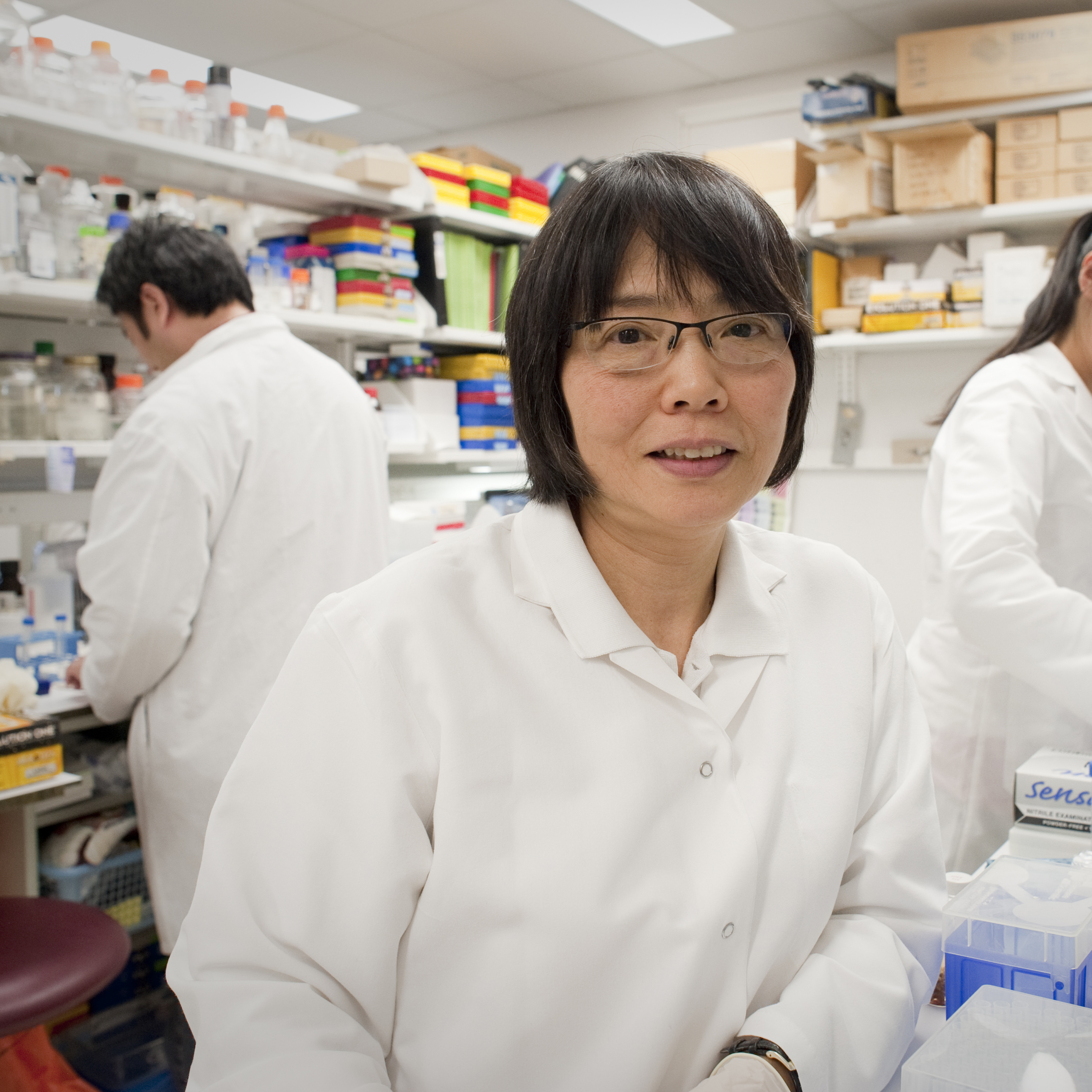
Shioko Kimura, Ph.D.
Dr. Kimura obtained her Ph.D. in chemistry at Hokkaido University, Sapporo, Japan. After postdoctoral studies at Queen's University, Kingston, Ontario and the National Institute of Child Health and Human Development as a visiting fellow, she moved to the Laboratory of Molecular Carcinogenesis, NCI. Since 1996, she has been head of the Endocrinology Section, Laboratory of Metabolism.
Dr. Kimura retired from CCR in June 2025.
News
Covers
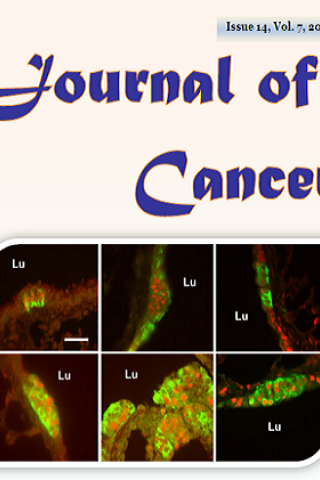
Co-expression of Achaete-Scute Homologue-I and Calcitonin Gene-Related Peptide during NNK-Induced Pulmonary Neuroendocrine Hyperplasia and Carcinogenesis in Hamsters
Cover: Co-expression of Achaete-Scute Homologue-I and Calcitonin Gene-Related Peptide during NNK-Induced Pulmonary Neuroendocrine Hyperplasia and Carcinogenesis in Hamsters
Abstract: Achaete-scute homologue-1 or ASCL1 (MASH1, hASH1) plays roles in neural development and pulmonary neuroendocrine (NE) differentiation, and it is expressed in certain lung cancers. This study was aimed to assess whether and/or how ASCL1 plays a role in 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK)-induced pulmonary NE hyperplasia and carcinogenesis in hamsters. Hamsters were injected 3 times weekly with either NNK or solvent alone (control) for treatment periods of 6 and 24 weeks, both without and with 6-week recovery. Immunohistochemical analysis was carried out to examine the expressions of ASCL1, CGRP (calcitonin gene-related peptide), secretoglobin SCGB1A1 (club [Clara] cell specific 10 kD protein, CC10, CCSP), synaptophysin (SYP), and PCNA (proliferating cell nuclear antigen). The number of ASCL1-expressing NE foci per airway increased from 0.8 in controls to 1.6 and 2.0 during NNK exposure for 6 and 24 weeks, respectively, and the number of cells per foci doubled after NNK exposure. Most ASCL1-expressing cells in NEBs (neuroepithelial bodies) were also CGRP immunoreactive; NNK enhanced this co-expression with CGRP, a NE marker with known proliferation-promoting properties. NNK also increased PCNA expression within NE foci. NNK-induced tumors showed no immunoreactivity for NE markers. This study confirms ASCL1 as an excellent marker for pulmonary NE cells and demonstrates CGRP co-expression in ASCL1-positive NEB cells participating in NNK-induced NE hyperplasia.
Co-expression of Achaete-Scute Homologue-1 and Calcitonin Gene-Related Peptide during NNK-Induced Pulmonary Neuroendocrine Hyperplasia and Carcinogenesis in
Hamsters. Naizhen X, Linnoila RI, Kimura S. J Cancer. 7(14): 2124-2131, 2016.