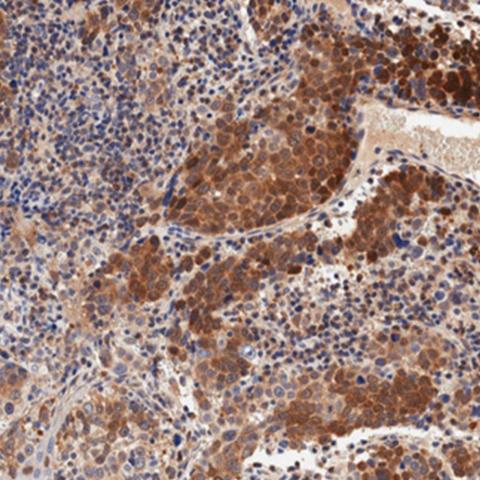
Researchers discovered that HPV-negative head and neck cancers can escape immunotherapy due to high levels of an enzyme called SMYD3. Seen in this image is a stain of HPV-negative head and neck squamous cell carcinoma that has high levels of SMYD3. Image credit: Saloura lab
CCR researchers have discovered one way that human papillomavirus (HPV)-negative head and neck cancers escape immunotherapy treatment. The finding, published July 17, 2023, in Cell Reports, holds promise for novel therapeutic approaches to help people with this disease.
HPV-negative head and neck squamous cell carcinoma is an aggressive cancer with poor prognosis. The cancer returns in nearly half of patients following treatment, and only about a fifth of HPV-negative head and neck cancers respond to immunotherapy — a type of treatment that enables immune cells to identify, seek out and attack cancer cells.
“A lot of research focuses on how to increase response to immunotherapy, because those patients who do respond can get a significant improvement in overall survival,” said Vassiliki Saloura, M.D., Ph.D., a Stadtman Investigator in the Thoracic and GI Malignancies Branch.
Her group wants to understand the role of proteins that regulate the structure and activity of DNA complexes called chromatin in the progression of HPV-negative head and neck cancer, including the mechanisms that make this cancer unresponsive to immunotherapy treatments. Importantly, the group wants to identify how these mechanisms can be reversed.
Saloura’s work focuses on specific enzymes that control the expression of large sets of genes by interacting with chromatin. In previous work, her group found that higher amounts of one such enzyme, called SMYD3, in head and neck cancer cells were linked to lower amounts of several small proteins, called chemokines, that can attract cancer-attacking immune cells to tumors.
In this study, Saloura’s team discovered that SMYD3 represses the expression of immune-related genes in response to signals from the immune system that are part of its natural defenses to germs and cancer. The ability to respond to these natural defense signals is an essential feature for cancers to be susceptible to immunotherapy. This unique biology, Saloura explained, may contribute to why HPV-negative head and neck cancers are so unresponsive to immunotherapy in some patients.
Accordingly, when the team depleted SMYD3 in a mouse model of HPV-negative head and neck cancer and administered immunotherapy, four out of eight mice experienced complete tumor shrinkage, and tumor sizes decreased in another two of the mice. In contrast, tumors continued to grow in all mice that received immunotherapy treatment alone without SMYD3 depletion.
“We’re sensitizing HPV-negative head and neck carcinomas in mice to immunotherapy treatment, and this holds promise as a novel therapeutic avenue for patients who have this disease,” Saloura said. A final finding in the study supported this possibility: tumors from patients with HPV-negative head and neck cancer with higher SMYD3 levels had fewer cancer-attacking immune cells and a poor response to the immunotherapy drug pembrolizumab.
Saloura hopes this work will establish the rationale for studying SMYD3 depletion in HPV-negative head and neck cancers in the clinical setting. The team’s next step is to identify and investigate potential pharmaceutical interventions that could degrade SMYD3 in these aggressive cancers in humans so that more patients can benefit from potentially life-saving immunotherapy approaches.