The rWTC-MBTA vaccine extended survival and prevented tumor recurrence in preclinical brain tumor models.
Raleigh McElvery, Scientific Communications Editor
March 8, 2024
Glioblastoma is the most common primary brain cancer in adults and remains one of the most challenging cancers to treat. People with these tumors usually undergo surgery, followed by radiation and chemotherapy. However, glioblastomas often resist treatment. For decades, there’s been little improvement in disease outcomes. The median length of survival is eight months, and the five-year relative survival rate is just 6.9 percent.
One problem is that the immune system doesn’t automatically view glioblastomas as a threat. In fact, it takes a lot to elicit an immune response in the brain. That’s because the stakes are high: If the body mistakenly attacks its own healthy tissue, the impact on brain function could be catastrophic. As a result, immune cells don’t usually target the tumor, allowing it to grow.
To boost the immune system’s response, researchers at the NCI Center for Cancer Research’s Neuro-Oncology Branch (NOB) have created a cancer vaccine that can activate immune cells to recognize and attack glioblastomas. In a recent study published in Advanced Science, they showed that their vaccine (called the rWTC-MBTA vaccine) could extend survival and prevent tumor recurrence in mouse models. Eventually, they hope this vaccine could supplement conventional treatments to improve care for people with glioblastoma.
The researchers previously tested their vaccine in preclinical models of breast cancer and melanoma, but this is the first time they’ve applied it to brain tumors.
“We were very excited to see how well the rWTC-MBTA vaccine performed in glioblastoma models,” says Zhengping Zhuang, M.D., Ph.D., the study’s senior author and head of the NOB’s Cancer Stem Cell Biology Research Program. “Our vaccine has the potential to enhance more traditional therapies to extend survival in people with glioblastoma. It could also be applied to address other hard-to-treat tumors.”
Boosting the Immune System to Attack Glioblastomas
Immunotherapies are treatments that harness the immune system to target tumors. At the moment, there are only a handful of immunotherapies being tested in clinical trials for brain cancers, including immune checkpoint inhibitors and CAR T-cell therapies. Although these immunotherapies show promise for treating multiple cancers, they have been relatively ineffective against glioblastoma. Immune checkpoint inhibitors are often unable to trigger an immune response because of the brain’s unique environment that suppresses immune cell activity. CAR T-cell therapies often fail because glioblastomas lack a universal identifying feature that the treatment can target across all tumors.
To address these limitations, many researchers are exploring cancer vaccines that help the immune system recognize and eliminate glioblastomas. One of these vaccines, called DCVax-L, was recently tested in a phase 3 clinical trial. Dr. Zhuang was inspired by this work and decided to create a vaccine that was less time-consuming and less expensive to produce.
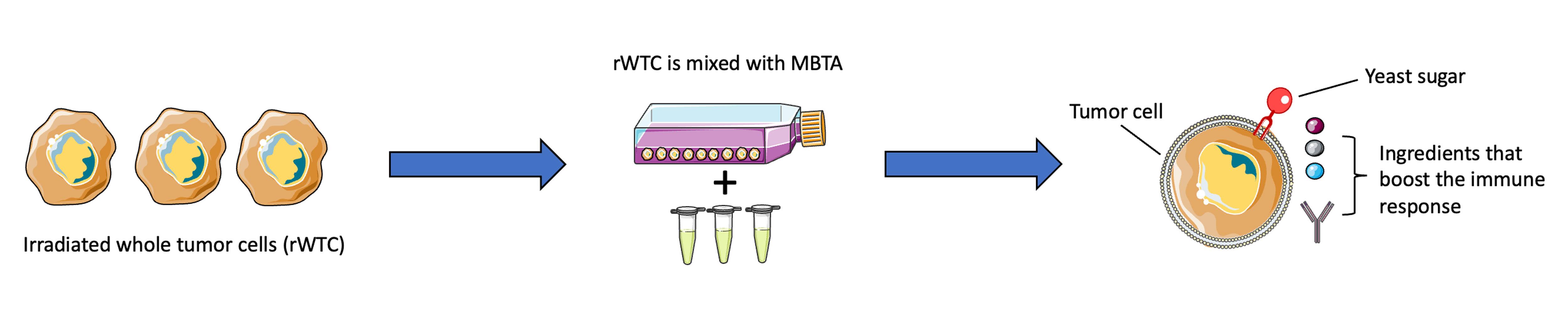
His team’s rWTC-MBTA vaccine contains two main components. The first, rWTC, stands for “irradiated whole tumor cells.” The researchers took glioblastoma cells and exposed them to enough radiation treatment that the cells could no longer grow, but not so much that they died immediately. The researchers then mixed the irradiated cells with the second component: MBTA.
MBTA consists of a cocktail of ingredients. One of them is a sugar found in yeast. During the mixing process, it becomes embedded in the irradiated tumor cells and acts like bait to attract immune cells, including one type called dendritic cells. The immune cells are drawn to it because they are programmed to kill microorganisms, including yeast.
The rest of the MBTA ingredients help to boost the immune system’s response once the immune cells home in on the irradiated cells. If the yeast sugar is the baited hook, then the rest of the MBTA components are the bucket of “chum” that draws even more curious fish. This two-pronged approach helps establish both innate immunity (an immediate, general immune response) and adaptive immunity (a more specialized and sustained response) against the tumor.
Other researchers have tried using MBTA alone to treat tumors. While this does boost the immune response, it doesn’t direct the immune cells to target glioblastomas specifically.
The study’s first author, NOB Staff Scientist Herui Wang, Ph.D., saw only modest results when he treated mouse models of glioblastoma with just MBTA. Treating them with just the rWTC component only had a weak effect as well. This indicated that both the rWTC and MBTA components were needed to initiate a potent immune response and improve survival. In fact, the cancer completely disappeared in seven out of 10 mice who received the rWTC-MBTA vaccine three times a week for four weeks. The vaccine even extended survival in a specific mouse model of glioblastoma that is highly resistant to immunotherapy.
“We were thrilled to see the brain tumors regress in our glioblastoma models,” Dr. Wang says. “In many cases, we were able to kill and remove the tumor instead of simply delaying growth by a few months. I hope the same outcome can be achieved in a clinical setting.”
The vaccine also helped prevent the tumors from coming back. After several months, the researchers reimplanted tumor cells back into the mice whose tumors had completely disappeared. This time, though, their immune cells remembered the tumor and stopped it from regrowing.
Advancing to Clinical Trials
Dr. Zhuang’s team is now making plans to help develop a clinical trial to test their rWTC-MBTA vaccine. The researchers hope to take tumor cells from the patient during surgery, treat the cells with radiation in the lab, combine them with MBTA, and inject them into the patient’s arm.
Dr. Zhuang believes their vaccine would be especially effective in combination with other conventional treatments. For example, it could be injected after chemotherapy to remove any residual tumor cells. It could also help convert immunogenically “cold” tumors that don’t trigger an immune response to “hot” tumors that allow immune checkpoint inhibitors to work. One of the next steps, the researchers explain, will be to test whether the brain’s protective blood-brain barrier affects the vaccine’s ability to reach the tumor site.
“Our vaccine is not a cure-all,” Dr. Zhuang says, “but it does have the potential to address the shortcomings in our current treatment strategies for glioblastoma—and hopefully prevent recurrence.”
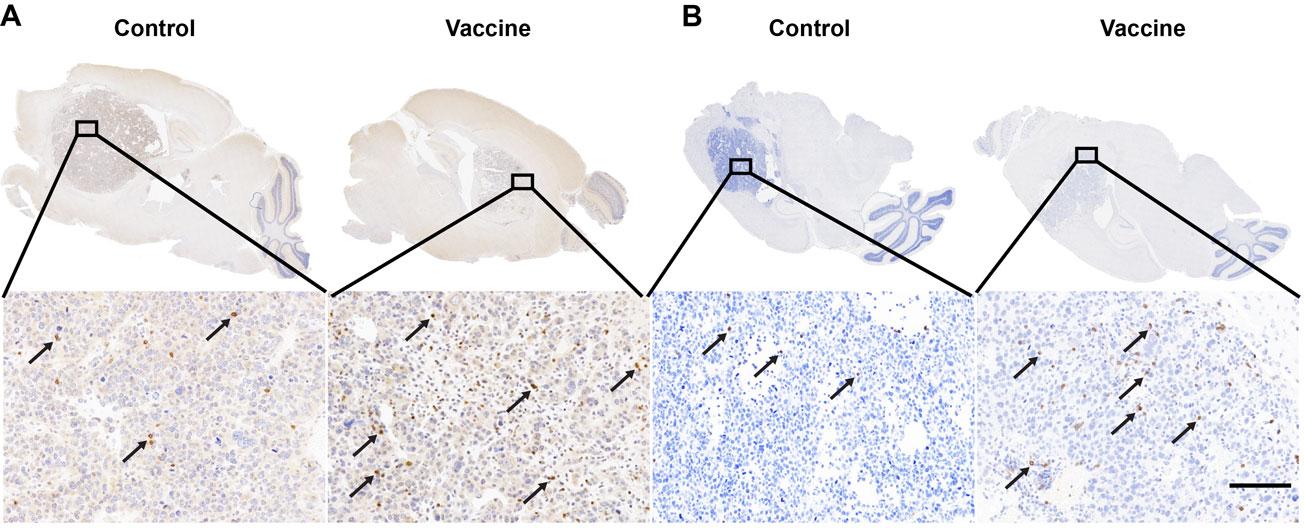
Top image caption: CD4 and CD8 staining results confirmed that immune cells called CD4+ T cells (A) and CD8+ T cells (B) are both increased in the brain tumors of the vaccine group. Credit: Courtesy of the researchers